What SLPs Need to Know:
Acquired Apraxia of Speech
10 min read
Producing speech is like taking a road trip. Your brain is the GPS, mapping out the route (motor planning), and your articulators are the car, carrying out those directions (motor programming). With acquired apraxia of speech, the GPS knows the destination, but the directions get miscommunicated, leaving the driver to make wrong turns, drive well below the speed limit, stall at green lights, and make countless U-turns. That’s the daily reality for people with apraxia when they try to get their message across.
Acquired Apraxia of Speech (AOS) is a motor speech disorder that involves impaired motor planning and programming. Unlike Childhood Apraxia of Speech, a developmental impairment, AOS can occur after an injury to the left cerebral hemisphere, like a stroke. AOS is one of three types of acquired speech-language disorders that speech-language pathologists (SLPs) diagnose, along with aphasia and dysarthria. Diagnosing AOS can be challenging, even for experienced SLPs.

To make it more complicated, patients can have concurrent speech-language diagnoses. Non-fluent aphasia commonly co-occurs with AOS, as well as unilateral upper motor neuron dysarthria after a stroke (Hybbinette et al., 2021). Clinicians must examine distinguishing features to help diagnose and prioritize treatment approaches, which is a challenge in itself.
Primary progressive acquired apraxia of speech (PPAOS), on the other hand, is associated with a neurodegenerative disease, not an acute injury (Utianski & Josephs, 2023). It’s associated with frontotemporal degeneration that occurs when there’s a buildup of 4-repeat tau protein. To learn more about PPAOS, visit the National Association of Aphasia website.
Diagnosing Acquired Apraxia of Speech
There isn’t one test that confirms or rules out AOS. The patient must meet specific diagnostic criteria in the speech assessment (Molloy & Jagoe, 2019). According to Wambaugh et al. (2006), the primary features of AOS include:
- slow, effortful speech
- dysprosody (i.e. equal stress pattern)
- sound distortions
- distorted substitutions
Duffy (2019) also notes that individuals with AOS have greater difficulty with sequential motion rates (SMRs) compared to alternating motion rates (AMRs).
Non-diagnostic characteristics of AOS can be found in aphasia without apraxia, so their presence alone does not indicate apraxia (despite what you may have learned in school years ago). These characteristics include:
- trouble initiating speech
- groping to find the right articulatory posture
- perseverative errors
- more difficulty with longer words
- self-correcting frequently, indicating error awareness
- easier automatic speech (e.g. counting, curse words)
- islands of error-free speech
There are also exclusionary characteristics, like normal or fast speech rate or typical prosody. If a person speaks normally or quickly, such as a person with fluent aphasia, they cannot have AOS.
The Apraxia Battery for Adults – 2nd Edition (ABA-2) can be used to diagnose and determine the severity of AOS. It takes about 20 minutes to administer and costs around $200 USD.
The Apraxia of Speech Rating Scale – Version 3.5 (ASRS-3.5) is a free 13-item scale with a 5-point scoring system to note the presence/absence of AOS features and the severity. A cohort study involving patients with neurodegenerative diseases found the ASRS-3.5 to have good interrater reliability and validity (Duffy et al., 2023).
Want a Printable Summary?
Unlock the Handout Vault
Dozens of high-quality, well-researched PDF handouts are available all in one place: The Tactus Virtual Rehab Center!
You’ll find a summary of this article, an Apraxia Treatment Guide, What is Apraxia? for patient education, a topic communication board, and more!
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
Access 50+ evidence-based treatments and 100+ handouts created specifically for adult medical speech-language pathologists.
Treating Apraxia of Speech in Adults
There are two broad categories of treatment for AOS that speech-language pathologists can implement:
Not a Medbridge member? Sign up with coupon code TACTUS for the best price to earn quality CEUs.
While more research on motor learning and apraxia treatment is needed, certain variables may offer superior results compared to their alternatives. These include:
- Intense practice: high number of trials, multiple days a week instead of limited trials once a week
- Distributed practice: a long treatment course (vs. massed practice)
- Variable practice: practice targets in different contexts (vs. constant practice in the same context)
- Random practice: practice targets in random order rather than blocked practice
- Feedback of results: feedback about accuracy rather than performance
- Low-frequency feedback: feedback after some trials, not all
- Delayed feedback: feedback after a short delay (e.g. 3 seconds) instead of immediately
Restorative Treatments for Acquired Apraxia of Speech
A 2023 systematic review by Munasinghe and colleagues groups restorative apraxia treatments into these three categories:
- Articulatory-kinematic treatments
- Rate and rhythm control
- Intersystemic reorganization
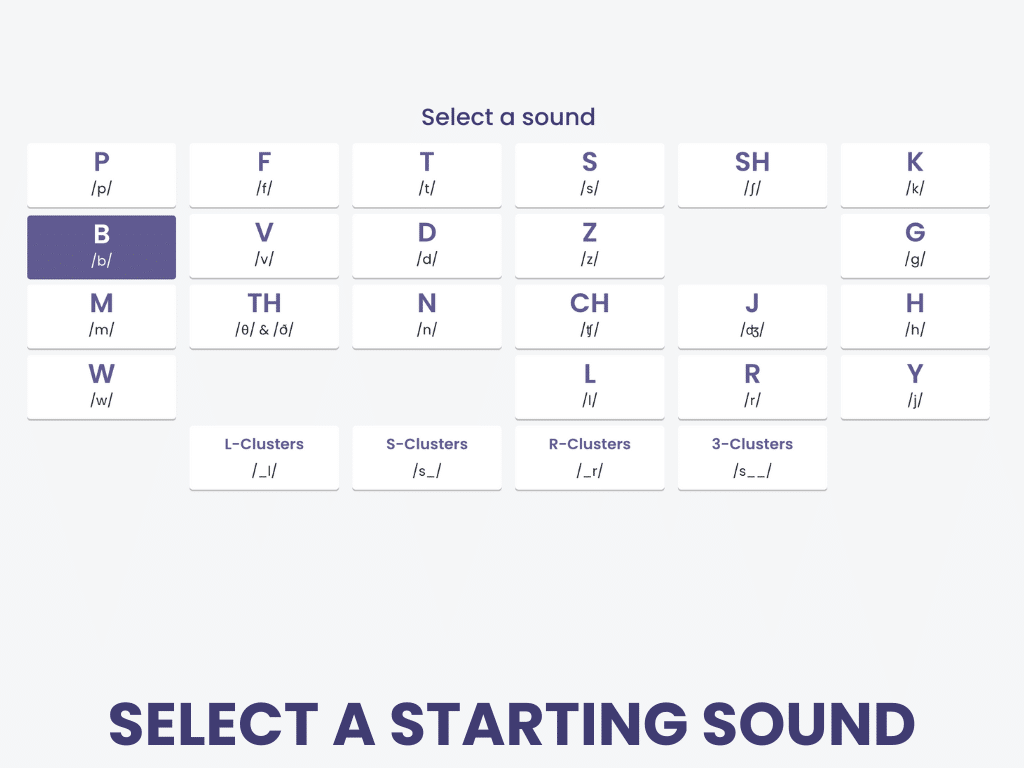
Virtual Apraxia Therapy:
Repeating Single-Syllable Words
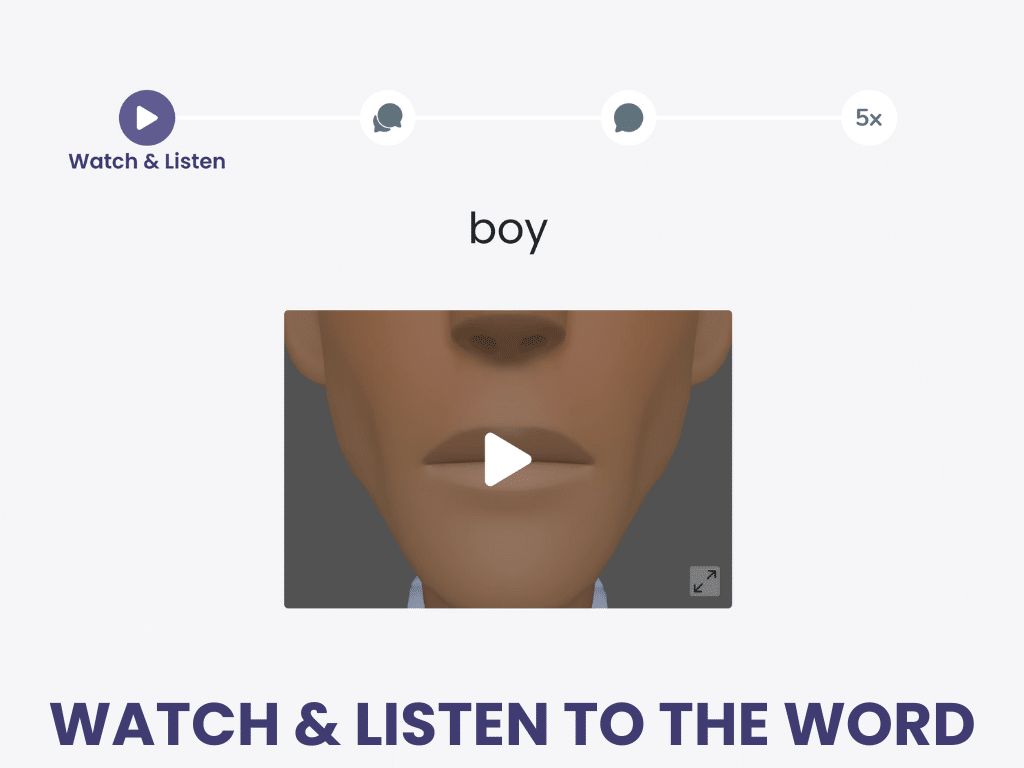
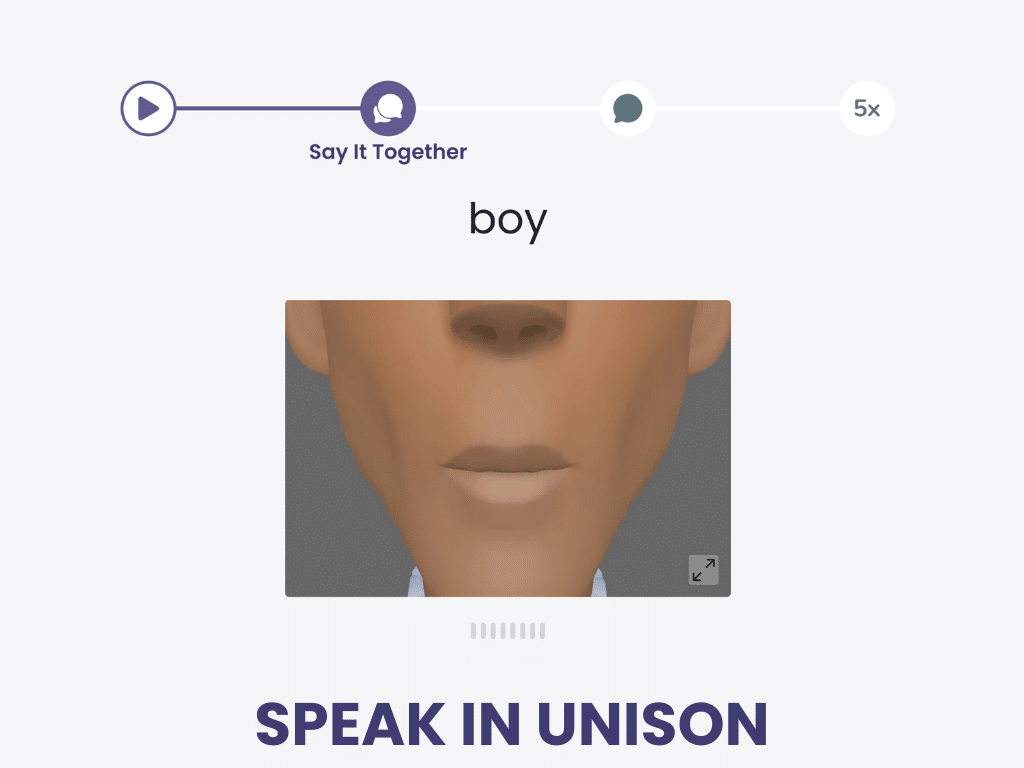
Repeating Single-Syllable Words is a talking treatment in the Tactus Virtual Rehab Center that uses integral stimulation to help people with apraxia say words beginning with each consonant sound.
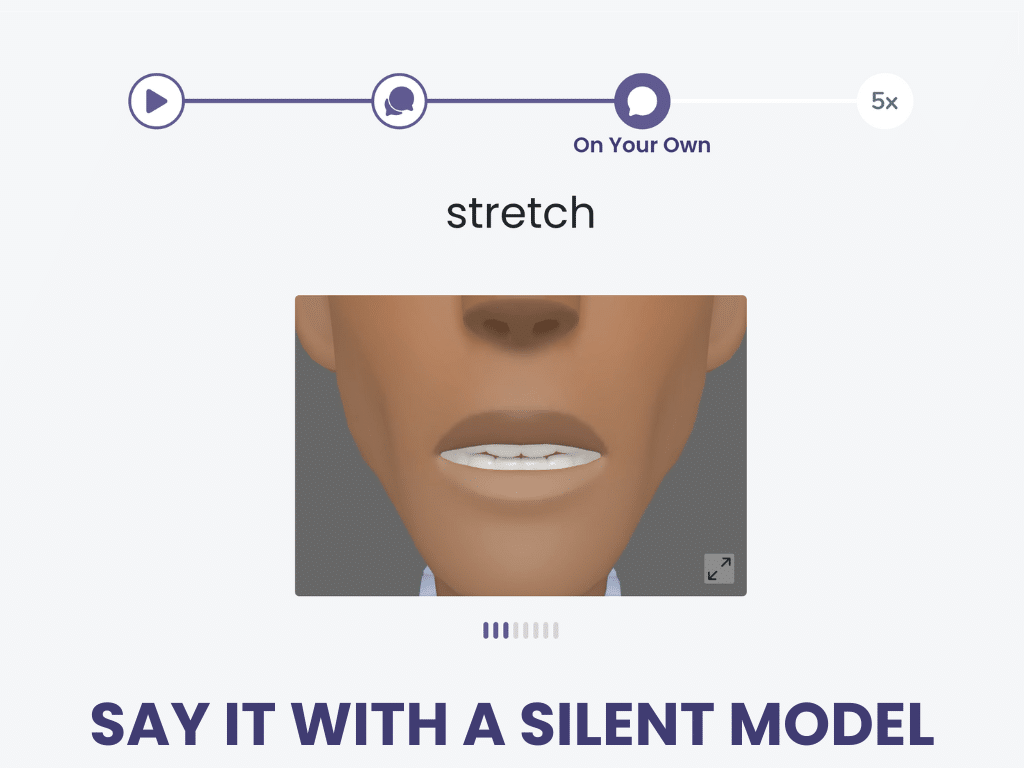
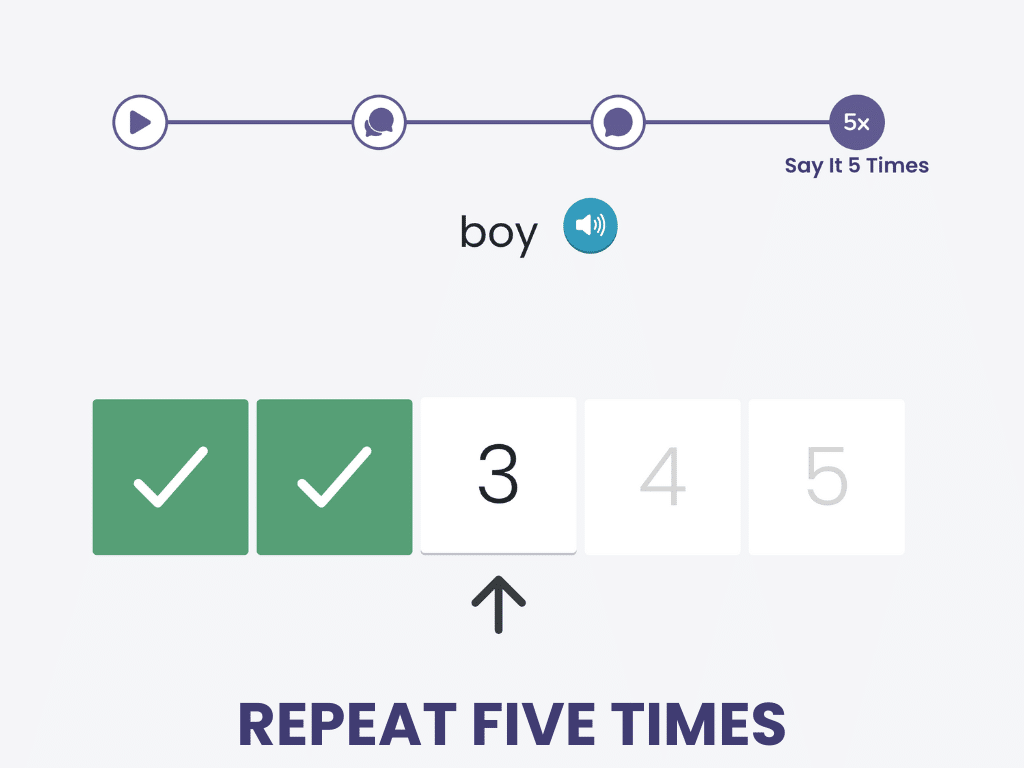
First, watch and listen. Then speak along. Say it on your own, then say it 5 more times.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
Use technology to help your patients get the intensive practice they need to relearn how to speak. Homework is free for patients!
1) Articulatory-Kinematic Treatments for Apraxia
Articulatory-kinematic (AK) treatments are the most researched of the three types of apraxia treatment. They target the spatial and temporal aspects of speech to improve articulation, motor planning, and sequencing (Mauszycki, 2011). This treatment approach is recommended for patients with sound errors across the spectrum of severity, including those in the chronic phase.
Articulatory-kinematic treatments include at least one of the following techniques to target speech production:
- Modeling: provide an auditory or visual example of the target (pretty standard)
- Integral stimulation: use the “Watch me, listen to me, say it together” framework, based on Rosenbek’s 8-Step Continuum
- Repetition: give repeated practice in a blocked order (e.g. soap, some, sing, set) or randomized order (e.g. sun, mop, boat, math, sit)
- Verbal feedback: provide feedback on the accuracy of the production (“That’s right” or “The initial /t/ sound wasn’t quite right, let’s try again”)
- Placement cues: provide verbal, visual, or tactile cues for the target sound (“Bite your bottom lip and blow air”)
- Minimal contrasts: enhance awareness of errors by comparing two words that differ by one sound, like came/game.
- Shaping: play to the patient’s strengths by taking a sound they can produce and shaping it into a different sound
- Visual feedback: use electropalatography or electromagnetic articulography to provide real-time visual feedback
How-To:
Integral Stimulation
It’s one thing to say you should use Integral Stimulation (IS), based on Rosenbek’s 8-Step Continuum, or Sound Production Treatment (SPT), but what exactly are those?
We’ve created a 4-page How-To guide to show you exactly what to do.
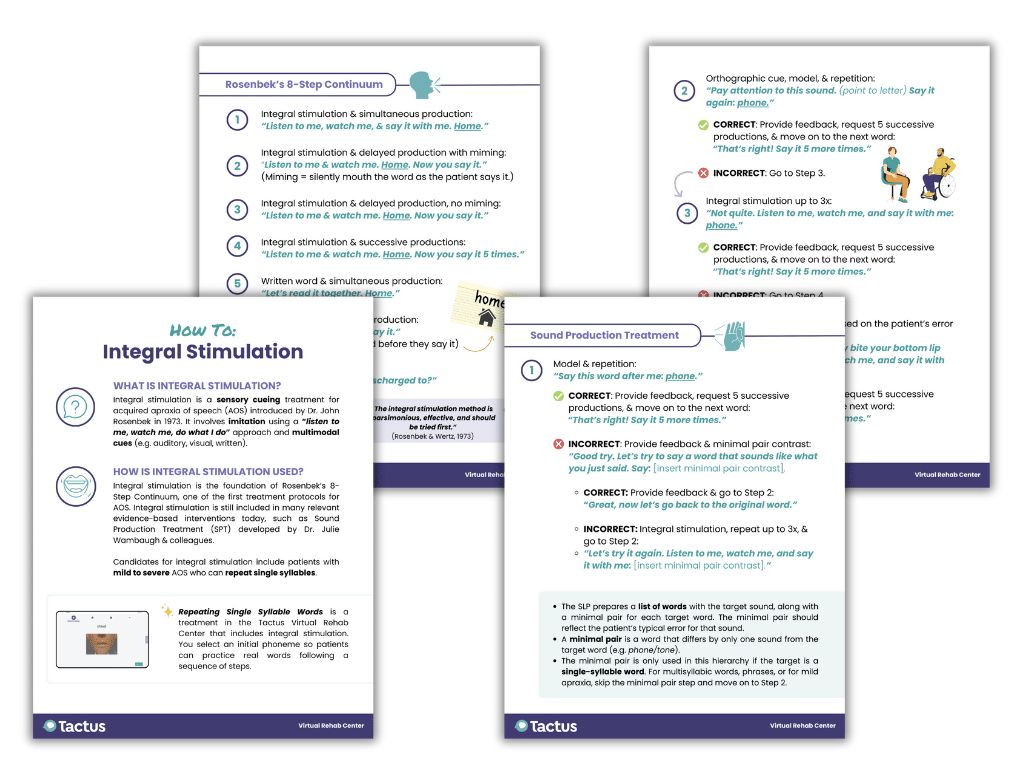
You’ll find this downloadable PDF handout in the Tactus Virtual Rehab Center. There are over 100 handouts in our vault, all for your use.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs to get access.
We know you want to help your patients in evidence-based ways. We’ll show you how.
There are several structured articulatory-kinematic treatment protocols, most of which use a hierarchy incorporating the above techniques. Keep in mind, there is no universal agreement that one AK approach is superior to the rest. Clinicians often combine techniques or approaches to maximize therapy outcomes.
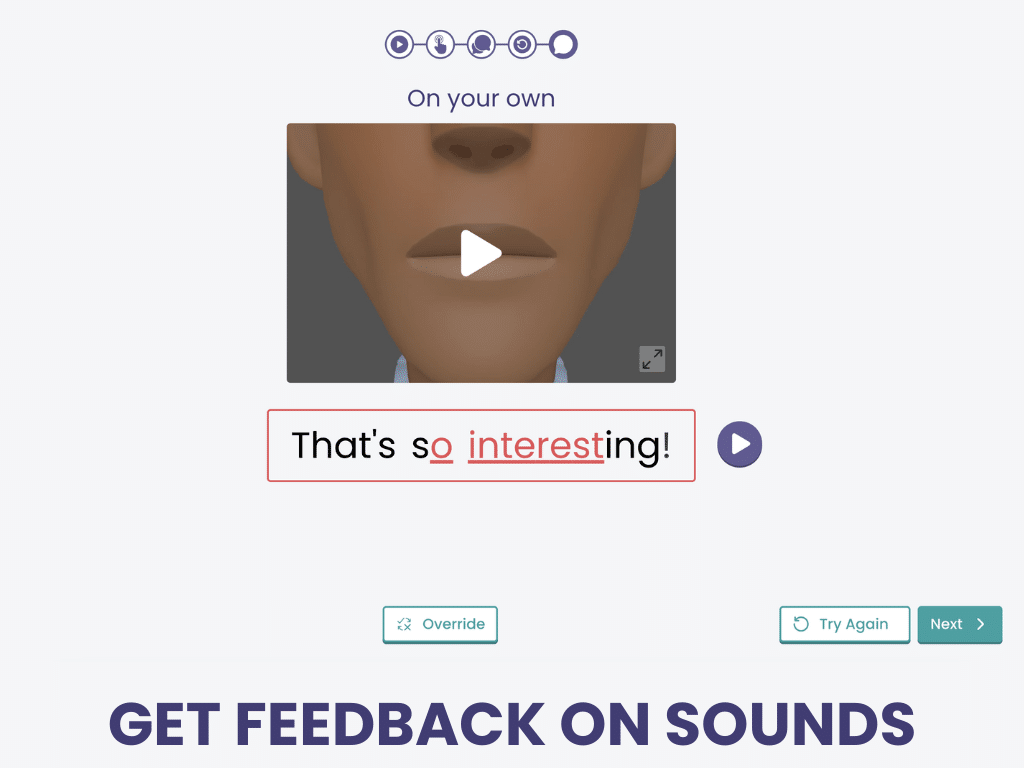
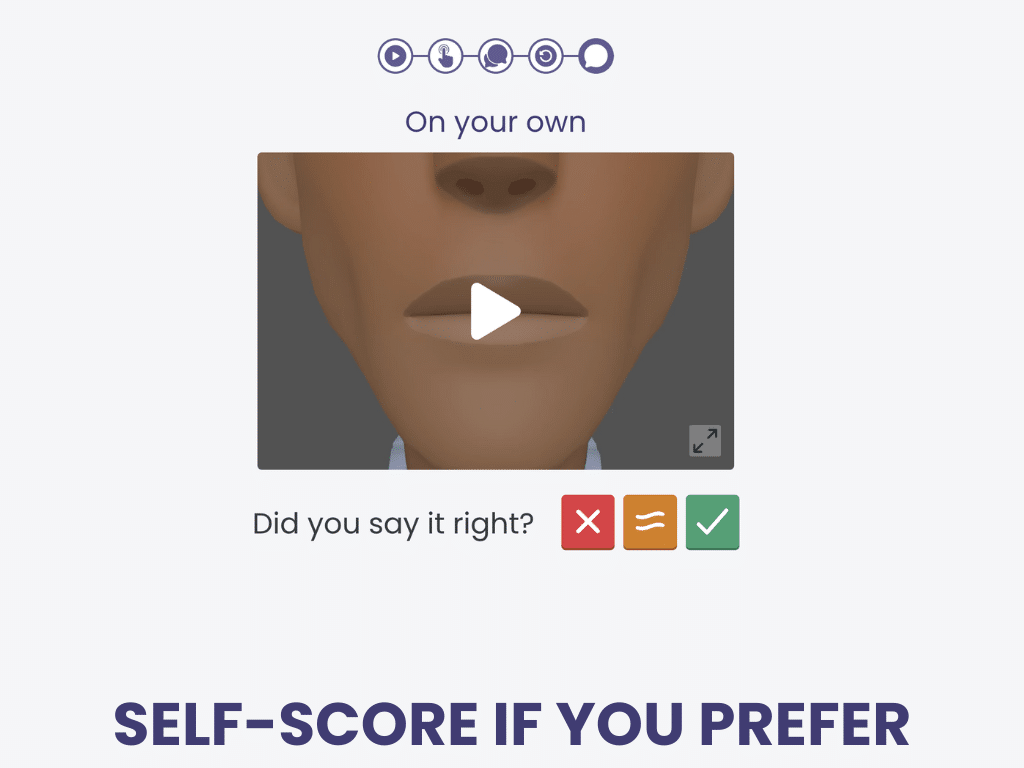
Ballard and colleagues (2019) found that feedback via automatic speech recognition resulted in improved word production accuracy for those with AOS. The Virtual Rehab Center has leveraged this technology for the treatment Repeating Single-Syllable Words. It integrates multiple AK techniques, including modelling using a realistic mouth model, placement cues, integral stimulation, and feedback using speech recognition.
2) Rate and Rhythm Control for Apraxia
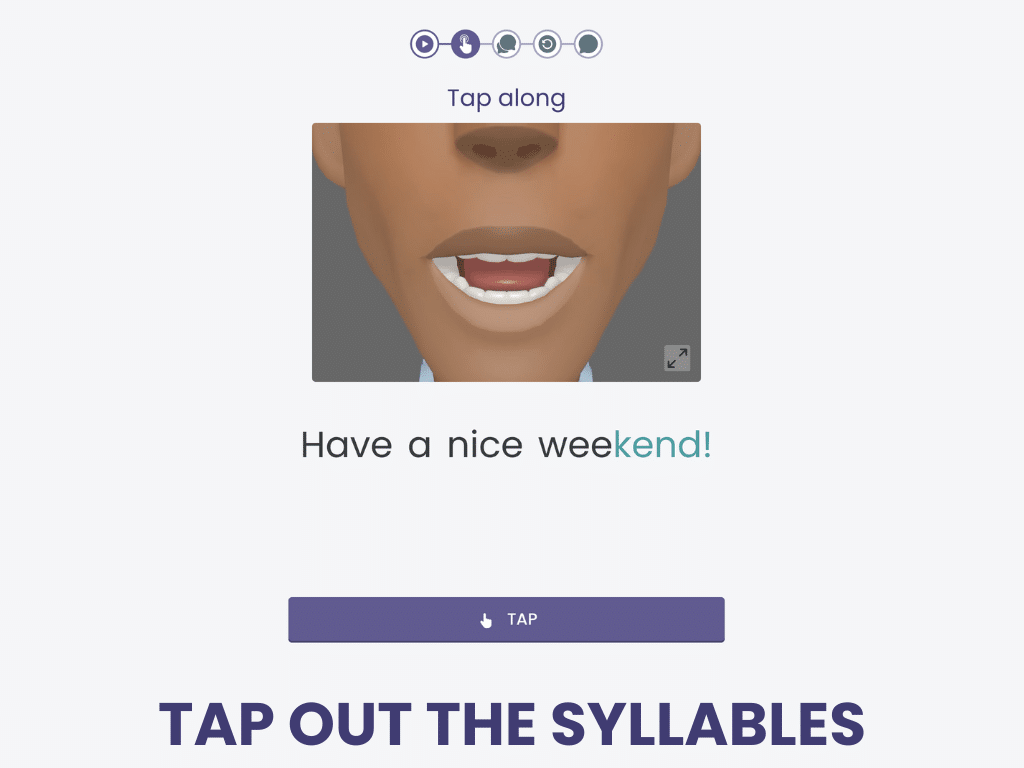
Another type of restorative treatment for AOS is rate and rhythm control, in which speech prosody (i.e. rhythm, melody, and intonation) is the primary focus. Treatments include pacing with a metronome (called metrical pacing), using a pacing board, or tapping a finger or hand along with syllables or words. Studies have found improved rate and sound production accuracy even though participants did not receive specific feedback about sound production (Ballard et al., 2015).
Virtual Apraxia Therapy:
Repeating Phrases
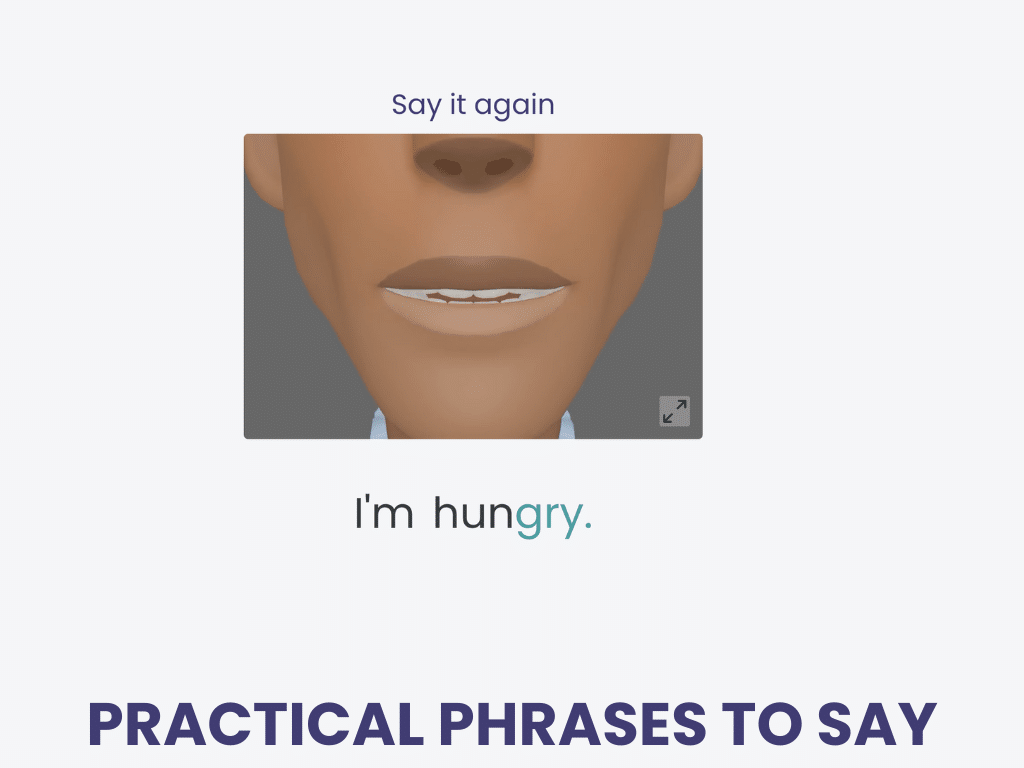
Repeating Phrases is a talking treatment in the Tactus Virtual Rehab Center to help adults with apraxia of speech.
It uses articulatory-kinematic approaches, including integral stimulation and finger tapping, to help people say the phrases that matter most.
Speech recognition provides sound-level feedback on accuracy, and a life-like avatar provides a realistic mouth model. Levels advance from 2 to 6 syllables.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
3) Intersystemic Reorganization of Apraxia of Speech
Intersystemic reorganization uses a patient’s intact system to facilitate speech, like incorporating singing in Melodic Intonation Therapy (MIT). MIT involves hand-tapping and saying functional words, phrases, and sentences with exaggerated intonation (i.e., singing). Utterances are first produced in chorus with the clinician, and then repeated.
Some papers classify MIT as a rate-and-rhythm approach, while others include it here because it leverages the brain’s right hemisphere. Most research focuses on the efficacy of MIT and Broca’s aphasia, so more research including participants with AOS is needed to support its effectiveness.
Other lesser-used intersystemic reorganization treatments include Speech–Music Therapy for Aphasia and rhythmic–melodic voice training, although these techniques also include rate and rhythm features, similar to MIT.
Selecting an Apraxia Treatment Approach
When choosing which restorative or compensatory treatments are best for your patient, consider these factors:
- Severity: Patients with mild AOS may use a few compensatory techniques, such as writing, but they wouldn’t benefit as much from low- or high-tech AAC as those with severe AOS would.
- Language skills: Some approaches (especially AK treatments) require adequate comprehension to interpret verbal cues or feedback. Those with impaired comprehension might benefit from supportive conversation techniques to support understanding, like using gestures or writing key words. Also, consider the reading and writing abilities required to use compensatory strategies. Language intervention may take priority over AOS treatment if impairments are severe.
- Hand mobility and praxis: Pointing to a communication book or a pacing board requires fine motor skills, as do writing, drawing, and gesturing, to be used effectively as communication strategies. Note the patient’s hand dominance and mobility before getting started. Be sure to assess for ideational and limb apraxia as well.
- Stimulability: Choosing sound targets for articulatory-kinematic treatments should depend on how stimulable the patient is. That is, can they produce the sound given a model, cues, and feedback? Choosing appropriate targets can help minimize patient frustration and allow for shaping similar sounds.
- Communication needs & lifestyle: Functional targets should always be considered. Whether it’s words, phrases, sentences, or whole scripts, try to choose stimuli that are meaningful to your patient. For example, if going to the salon is part of a patient’s routine, you might use a script to schedule a manicure.
- Patient buy-in: Unfortunately, motor speech exercises don’t always get the same buy-in that physical exercises get. If your patient is skeptical about a particular approach, their participation, motivation, and home practice will suffer. Educating patients and families about the rationale and research behind an approach can help, as can involving them in the selection of stimuli and treatments.
Remember, it’s okay to pivot if a treatment method isn’t working out. Use your best clinical judgement and always return to the evidence.
Learning More about Acquired Apraxia of Speech
We used many references to bring you this information, all linked where cited. We recommend these selected sources for a good overview:
Cite this article: Shahid, S. (2026, January). What SLPs Need to Know: Acquired Apraxia of Speech. Tactus Therapy. https://tactustherapy.com/ acquired-apraxia-of-speech-therapy-guide-slp/