What SLPs Need to Know:
Awareness
12 min read
Imagine being back home months after a brain injury, thinking life should be returning to normal. You cook dinner as usual, but you leave the stove on. You get lost driving to a familiar place and snap at a loved one for offering help. Everyone around you seems overly cautious, constantly pointing out mistakes you don’t even realize you’re making. To you, things feel fine—but your independence is slowly being taken away, and you don’t understand why.
Impaired self-awareness is the inability to recognize your own strengths and limitations after a brain injury. A similar condition is called anosognosia, which is used to describe reduced awareness of a specific impairment, like left neglect after a right-hemisphere stroke (Blake, 2018). According to Mamman and colleagues (2022), up to 97% of those with moderate to severe traumatic brain injury (TBI) experience reduced awareness. This is caused by a combination of physical and psychological factors (Terneusen et al., 2023) and is influenced by a person’s emotional state, culture, and values (Fleming & Osworth, 2006).
People with reduced awareness often don’t realize they need extra help. As a result, they might resist speech therapy because they don’t think there’s anything to work on. Motivation is a key factor to recovery, and it would be very difficult to stay motivated if you don’t understand why you’re in speech therapy in the first place. Much of cognitive-communication treatment is strategy instruction; again, why bother to learn or use a strategy if you don’t think there’s a problem?
Most studies confirm that poor awareness negatively impacts therapy outcomes (Robertson & Schmitter-Edgecombe, 2015). A systematic review by Dromer and colleagues (2021) reported that most studies “found poor self-awareness associated with poor rehabilitation, functional, social and vocational outcome and with increased burden on relatives.” Without insight, a person’s safety and independence are at risk.
Assessing Awareness
Given the potential impact, clinicians should assess awareness during the evaluation and address it early in the treatment process. A survey by Winkens et al. (2014) confirmed that clinicians know it’s important to evaluate awareness, but only a small number actually use a specific measure.
Consider the Awareness Questionnaire (AQ) or the Patient Competency Rating Form (PCRF) to look at awareness. Both free self-reported outcome measures include a patient rating form, a family member rating form, and a clinician rating form. Compare responses to get a patient-proxy discrepancy score: the difference between the patient’s score and that of the family member. The size of the discrepancy can provide insight into their awareness deficits (Dromer et al., 2021).
Clinician-led interviews, like the Self Awareness Deficits Interview (SADI – PDF), are another way to assess awareness. These measures, along with clinical observation, can not only identify a self-awareness impairment, but they can also point to broader executive dysfunction and social-behavioral challenges.
If awareness is intact, look out for signs of anxiety and depression. Awareness and mood have an inverse relationship— better awareness might mean higher emotional distress (Dromer et al., 2021).
Looking for Printable Resources?
Unlock the Handout Vault
Dozens of high-quality, well-researched PDF handouts are available all in one place: The Tactus Virtual Rehab Center!
Patient education, home practice, clinical guides, visual supports, & a summary of this article for quick reference.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
Access 50+ evidence-based treatments and 90+ handouts created specifically for adult medical speech-language pathologists.
Models of Awareness: Enter Metacognition
It’s useful to be aware of the awareness models to recognize a patient’s challenges and write targeted goals. Crosson and colleagues proposed an early “pyramid” model of self-awareness in the late 1980s (Robertson & Schmitter-Edgecomb, 2015) that included three levels:
- Intellectual awareness: You recognize the impairment (“My memory isn’t the same since the accident”)
- Emergent awareness: You can monitor performance and recognize problems as they happen, but you don’t anticipate problems ahead of time (“I know I’m missing an ingredient, but I can’t think of what it is”)
- Anticipatory awareness: You predict challenges that could arise because of the impairment (“I’ll make a grocery list and cross things off as I go. This way I won’t forget anything.”)
The more recent Dynamic Comprehensive Model of Awareness (DCMA) proposed by Toglia & Kirk takes metacognition (thinking about your own thinking) into consideration. Toglia & Goverover (2022) revisited this topic in a recent scoping review. The DMCA involves two types of awareness:
- Offline awareness (or metacognitive awareness/knowledge)- preexisting knowledge of your cognitive strengths and weaknesses, the demands of a task, and strategies to help you succeed. Offline awareness is similar to intellectual awareness from the pyramid model.
- Online awareness– assessing a situation during a task and changing your perception after the task. This is called self-monitoring, and it’s comparable to emergent and anticipatory awareness. Self-monitoring includes error monitoring (recognizing mistakes) and self-regulation (changing performance).
O’Keefe and colleagues (2007) found that good error monitoring was associated with “less anxiety, less impairment of frontal behaviours, and better overall competency” in participants with traumatic brain injury (Robertson & Schmitter-Edgecomb, 2015). Clinicians should take note of error-monitoring during the initial assessment for a real-time sense of their awareness.
Treating Awareness to Build Insight
Recognizing the underlying factors that contribute to impaired self-awareness can help clinicians choose the right treatment. According to Fleming & Osworth (2006), there are three factors to consider:
This means it’s not just the brain damage that contributes to the lack of awareness. Someone who is naturally stubborn might refuse to accept their impairments. Someone might not be willing to give up their independence because of cultural norms. Dig deeper into the why to help narrow down the best treatment approaches for the individual patient. Here are some research-backed interventions you can use (scroll down to learn more about each one):
- Motivational Interviewing
- Meta-Therapy
- Patient Education
- Metacognitive Strategy Training
- Structured Feedback
1) Motivational Interviewing
Clinicians can use motivational interviewing for individuals with awareness deficits. This approach involves collaboration, patient autonomy, self-efficacy, and patient-centered goal setting (Medley & Powell, 2010). Clifford (2023)wrote a useful summary of tips for healthcare workers, such as:
- Use active listening (paraphrase and validate feelings)
- Provide affirmations to improve confidence
- Ask for permission before giving advice
- Ask for their ideas and opinions
In a randomized controlled trial, Bell et al. (2005) found that clients with TBI who participated in motivational interviewing improved in functional and subjective quality of life outcomes compared to a control group.
2) Meta-Therapy for Cognition
Similar to motivational interviewing, Tilton-Bolowsky et al. (2023) brought “meta-therapy” from the voice therapy space to cognitive-communication. A key component of meta-therapy is effective clinical dialogue, or how clinicians speak to their patients. The goal is to “get client buy-in, increase engagement, and improve treatment efficiency and outcomes more broadly.” Some fundamental rules of meta-therapy include:
- Treatment rationales should be clear and in plain language.
- Link therapy activities to real-life behaviors.
- Be specific about actions you’ve observed instead of focusing on accuracy alone.
- Let the patient’s responses to your dialogue or treatment approaches guide what to do next- be flexible.
3) Patient Education about Awareness
Build awareness by taking the time to educate patients about their brain injury – how it affects thinking, emotions, and daily life (Cicerone et al., 2022). When patients feel respected, informed, and included in their own recovery process, they’re often more willing to self-reflect. Use patient-friendly visual supports during this discussion.
Find a patient-friendly handout about awareness in the Resource Vault in the Virtual Rehab Center!
Focus on symptom indicators (e.g., forgetting appointments, losing track of time) instead of labels, like “executive dysfunction.” Remember to validate the patient’s feelings about the difficulties they’re experiencing since their injury (“Yes, it is stressful arriving late to work every day. That must be hard for you.”)
Keep in mind, not all patients will respond positively to education, especially those with denial or a defensive personality (Fleming & Osworth, 2006). In these cases, a behavioral approach might be best (Bieman-Copland & Dywan, 2000). This involves educating the patient on coping strategies (like relaxation techniques) before working on behaviors, and counseling to acknowledge the grief surrounding their injury.
If socio-cultural and environmental factors play a role in a patient’s unawareness, then educational groups, support groups, and peer mentoring programs are recommended, in addition to clinician-led education.
Build Awareness Step-by-Step:
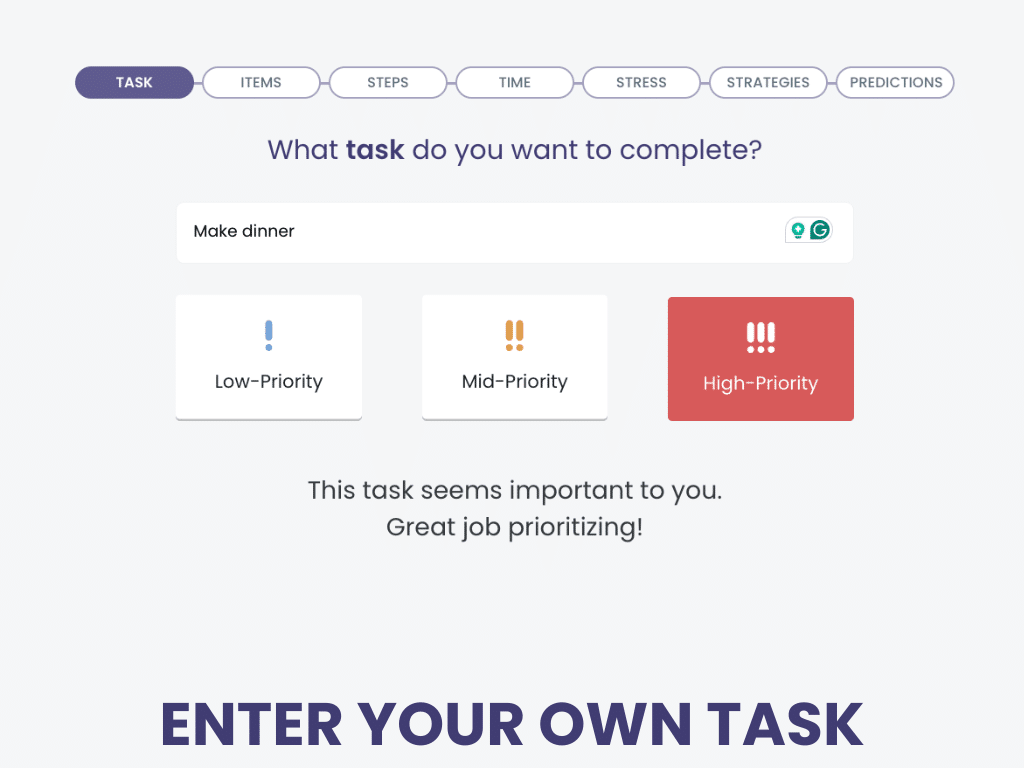
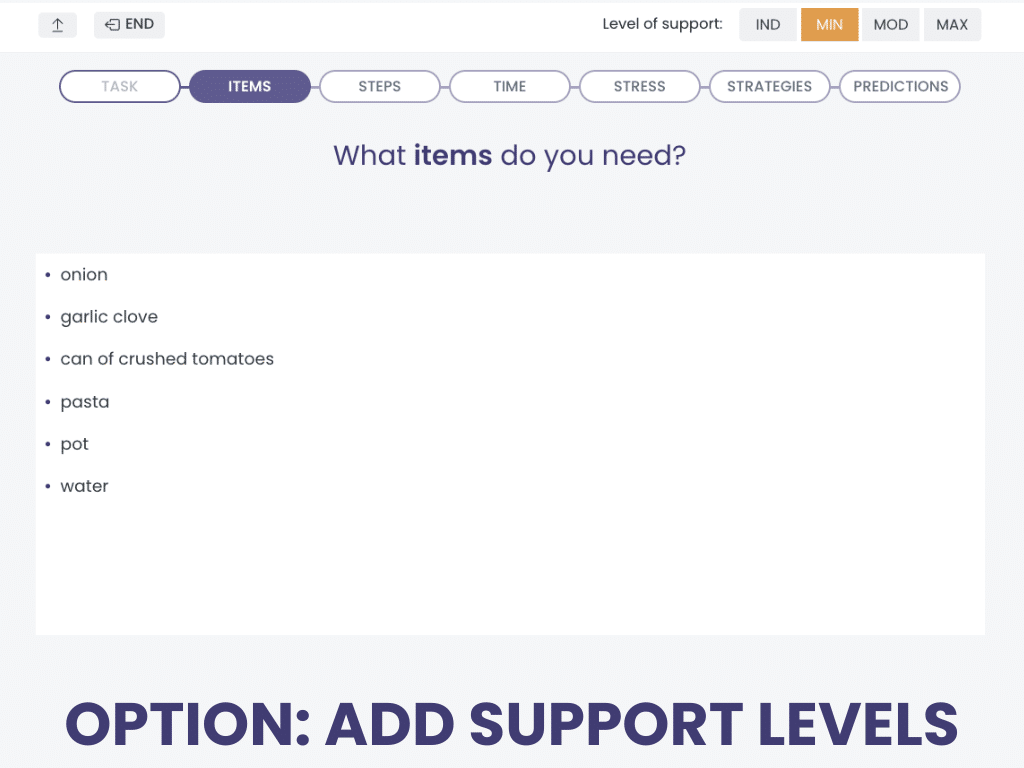
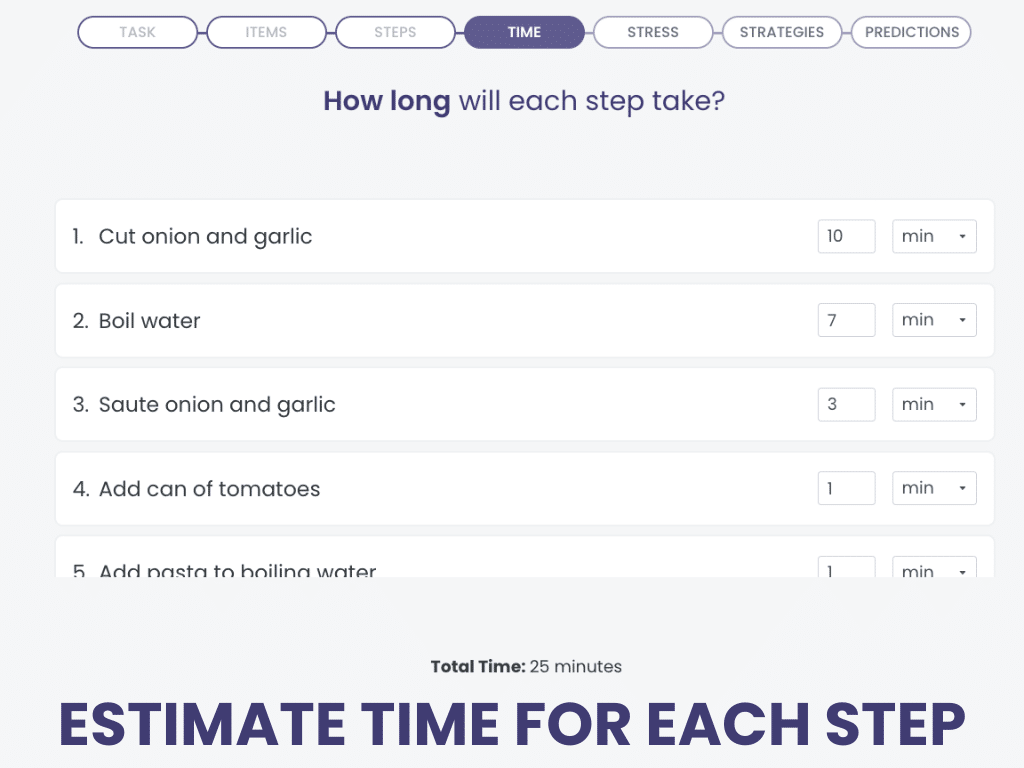
Planning Your Tasks
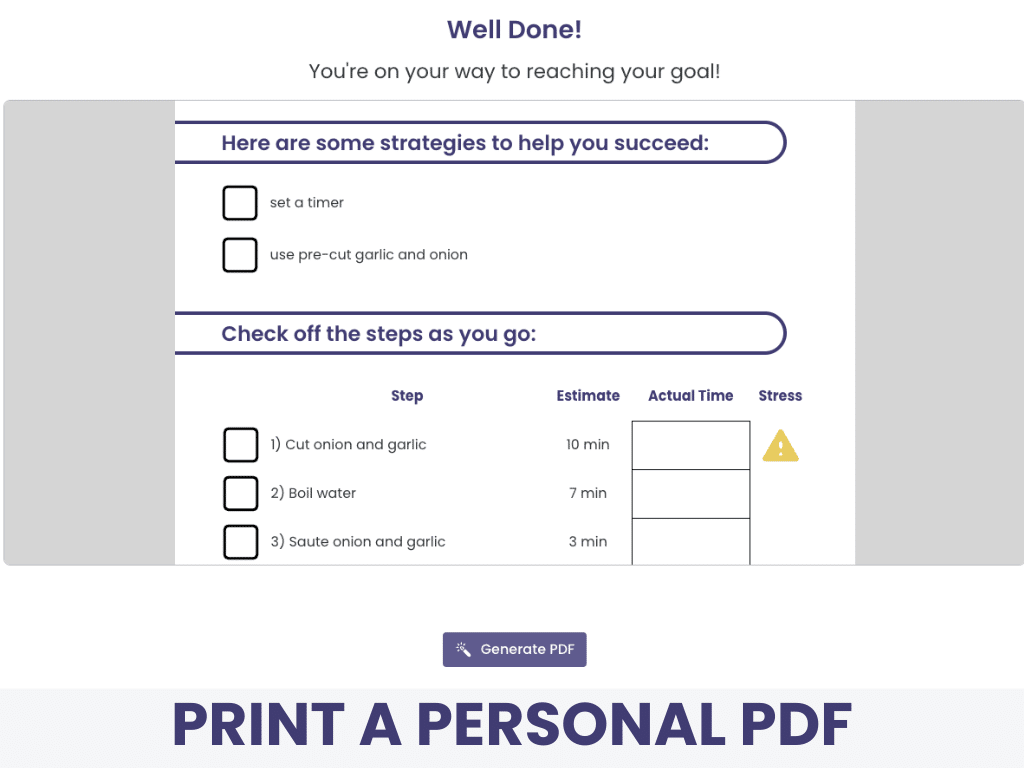
Planning Your Tasks is a cognitive treatment in the Virtual Rehab Center that works on awareness and executive functioning.
Work through planning, executing, and reflecting on a personally meaningful task, step by step in our 7-part sequence.
Planning Your Tasks gives you a printable PDF at the end of the treatment to allow for follow-up after the task has been completed.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
We know that awareness is personal, which is why this task is all about succeeding at something motivating in real life.
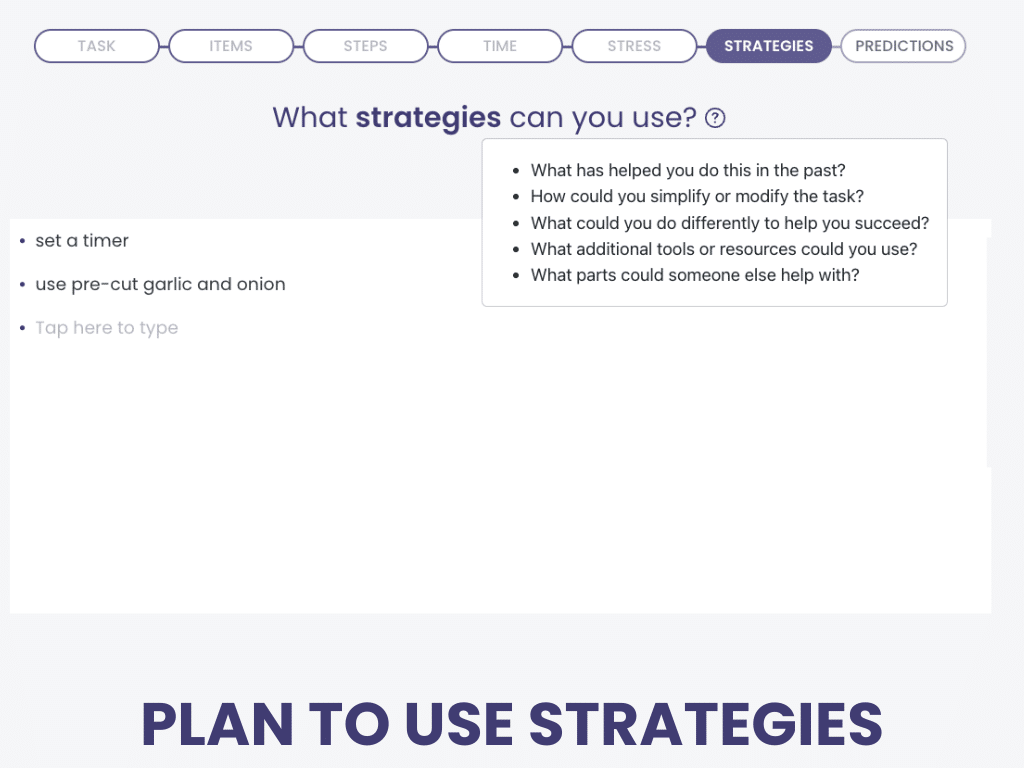
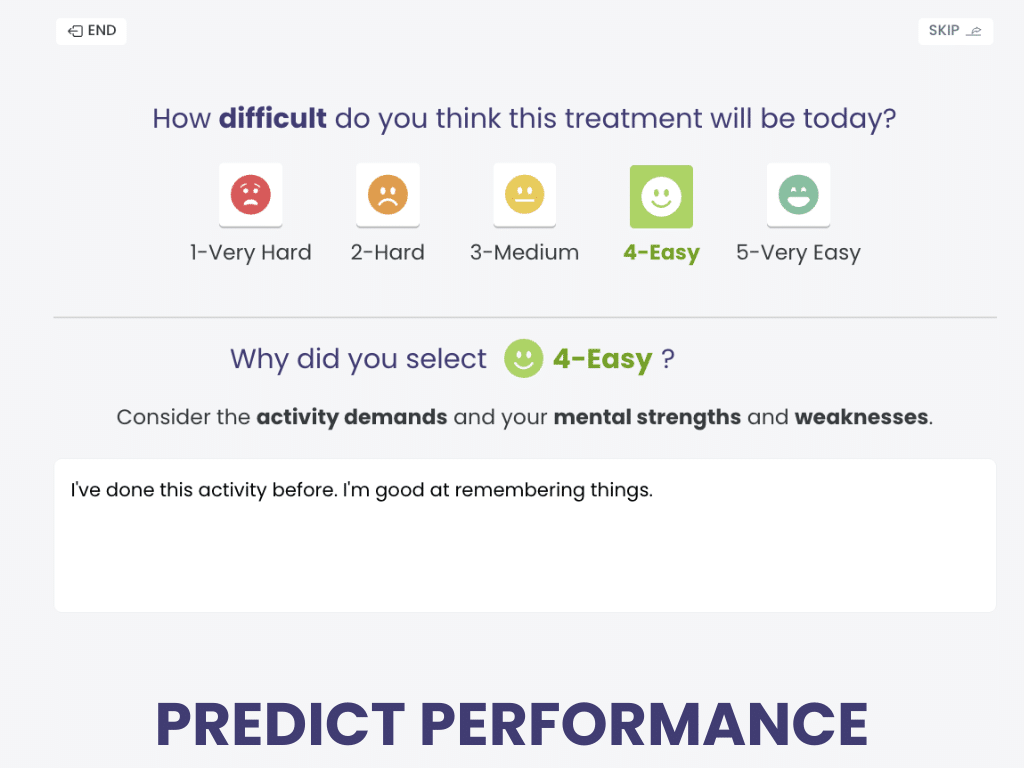
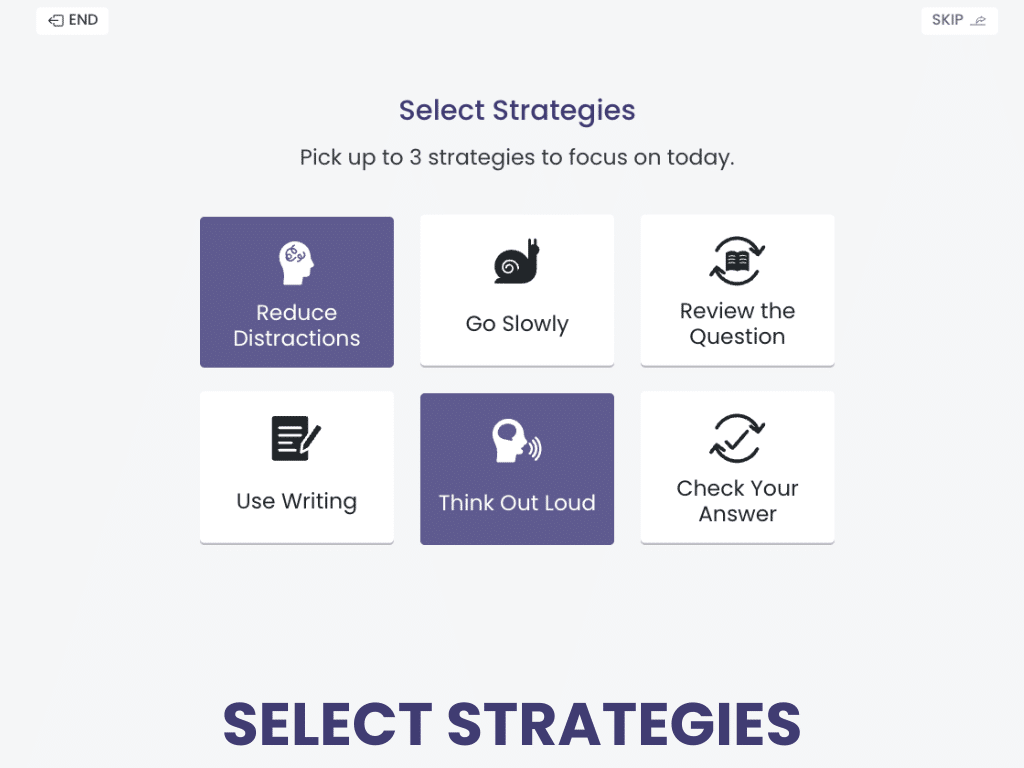
4) Metacognitive Strategy Training (MST)
Any metacognitive approach that involves self-monitoring and feedback can be used to address awareness (Jeffay et al., 2023). Providing these opportunities in structured, familiar tasks can help patients redefine their offline awareness– general knowledge about their own abilities (Fleming & Osworth, 2006). This process is generally referred to as “guided mastery” in the literature (Toglia & Goverover, 2022).
Clinicians can and should vary the actual tasks (e.g., enrolling in a class, filing documents, arranging childcare), but the learned metacognitive procedure should be constant to help make the process a habit (Fleming & Osworth, 2006). Try to choose tasks that will elicit errors to target awareness (Blake, 2018).
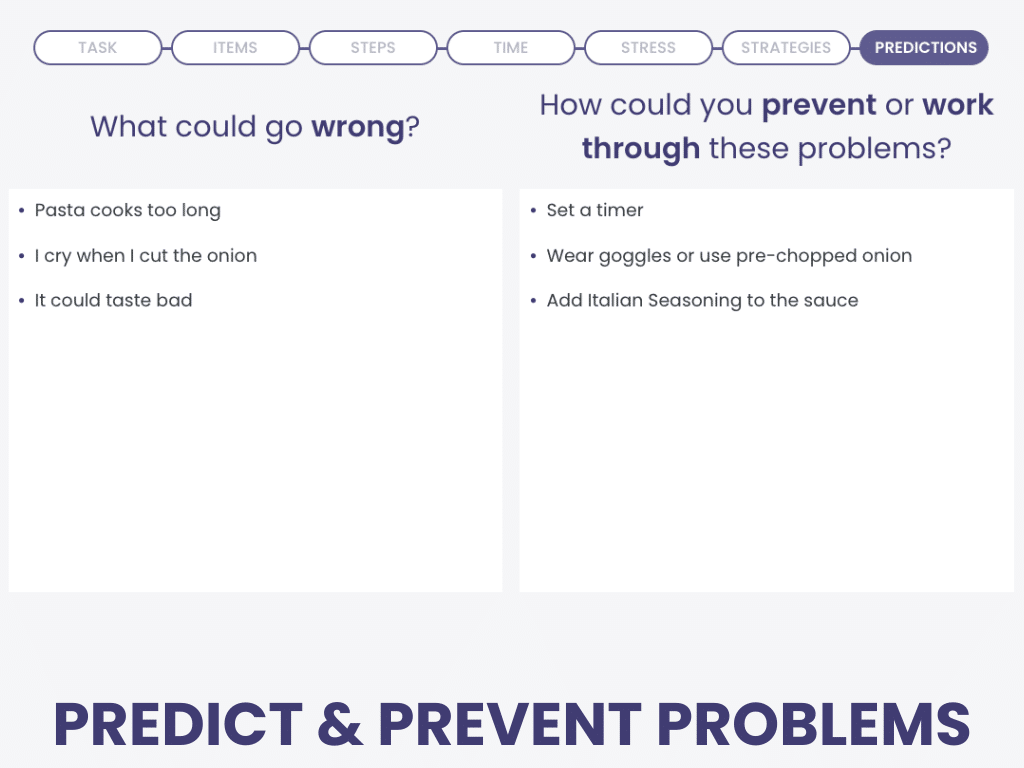
Metacognitive procedures usually include these elements before, during, and after a task:
There are two evidence-based treatments, Awareness Training and the Predict-Perform-Evaluate procedure, that include similar steps to improve awareness and address executive dysfunction.
Let’s take the task of packing a suitcase as an example. The patient would follow these steps:
| STEPS | EXAMPLE |
| Define performance goals | Pack 5 appropriate outfits and hygiene items in 40 minutes. |
| Predict performance about difficulty, potential obstacles, number of errors, accuracy, speed of completion, etc. | It will be easy to pack the suitcase. I think I can pack in 30 minutes. I might forget 1 or 2 items. |
| Anticipate and plan for obstacles or errors. | I could forget something, or items might not fit. |
| Choose at least one strategy to reduce the chance or errors or prevent obstacles. | I could use a checklist, talk out loud, or set a timer. |
| Assess how much help they might need. | I will ask my partner to help fold the clothes. |
| Perform the daily living task. | Pack the suitcase. |
| Self-assess performance. This could be in the form of a structured interview or questionnaire. | I did not forget anything, but it took over an hour. It was harder than anticipated. I get tired easily since my injury. |
| Receive feedback from the clinician and compare their assessment with your observations. | I forgot the sunscreen and toothpaste after I abandoned the checklist halfway through. |
| Record their experience by writing a reflection or journal. | I’m having trouble staying organized. If I become more consistent with using a checklist, I won’t miss anything. Next time I can take a few short breaks, so I don’t get as tired. |
In a randomized controlled trial, Goverover and colleagues (2007) found that the experimental group that received Awareness Training improved in self-regulation and performance during instrumental activities of daily living (IADLs). These changes were not reflected on the Awareness Questionnaire, so further studies are needed with larger groups and more treatment sessions.
Predict-Perform-Evaluate
Built Into Cognitive Treatments
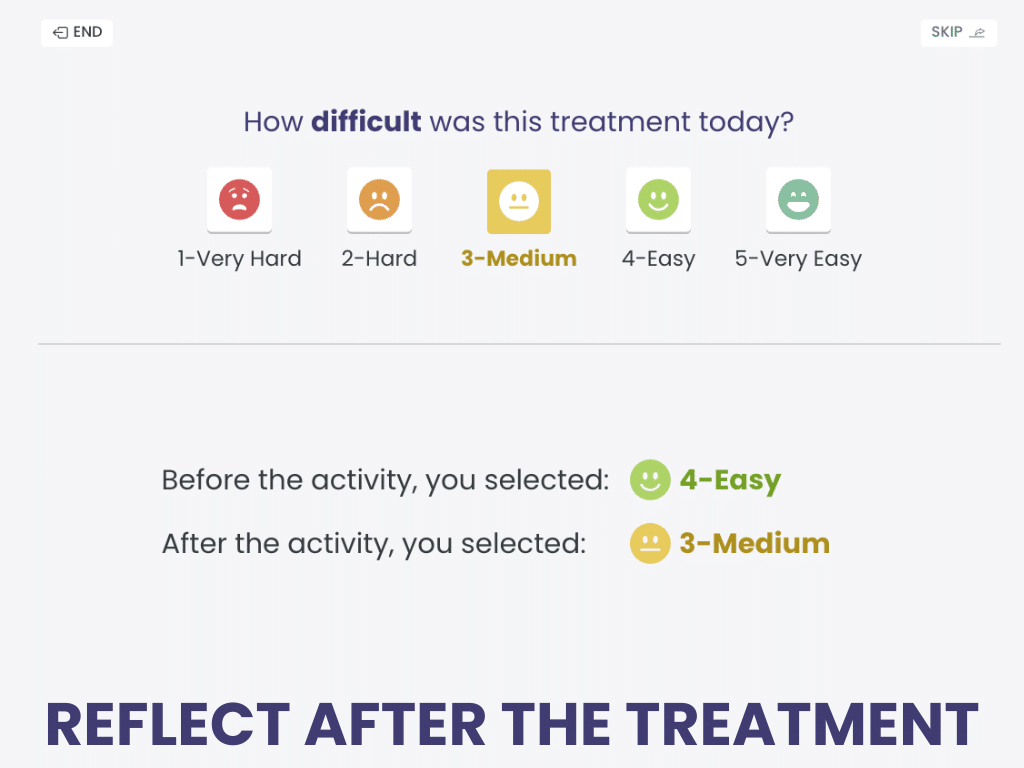
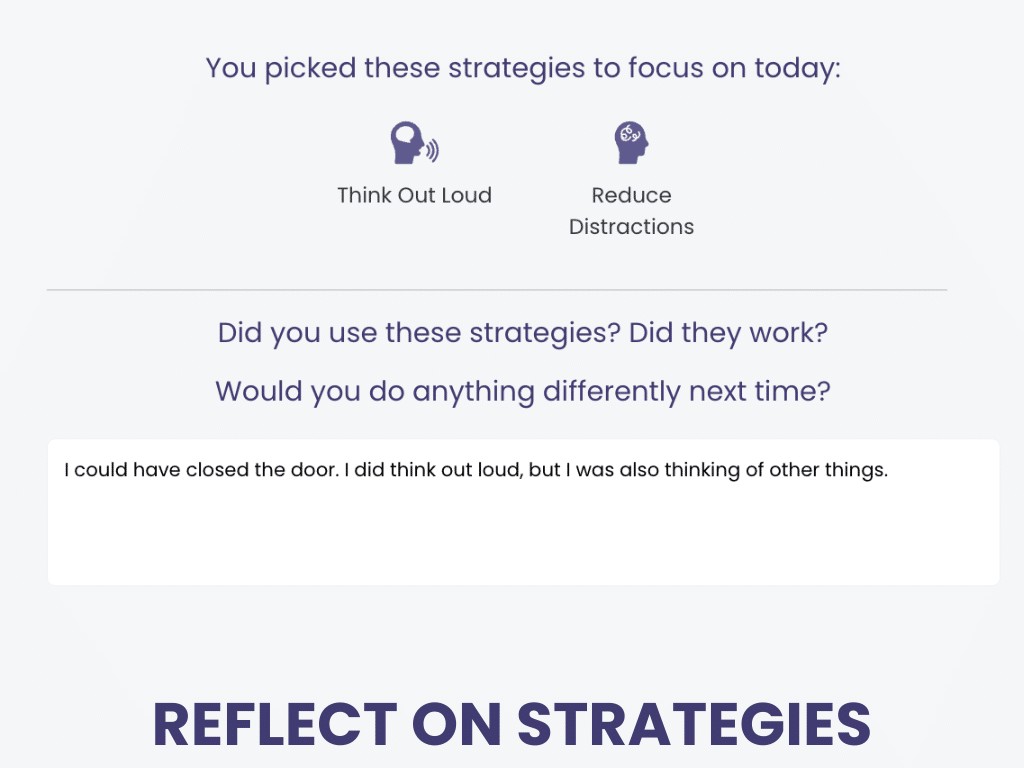
The Metacognitive Framework is something you’ll find wrapped around most cognitive treatments in the Tactus Virtual Rehab Center.
Before starting, patients predict their performance and choose strategies. After completing, they reflect on their prediction and strategy usage.
Making best practices easy is what the Virtual Rehab Center excels at. You don’t have to remember to ask and reflect – it’s built right in.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
5) Providing Structured Feedback
According to the INCOG 2.0 guidelines (2023), feedback is key to improving error recognition and overall awareness during everyday tasks. In a randomized controlled trial, Schmidt et al. (2013) found that combining verbal and video feedback was better than verbal feedback or experiential feedback alone for participants with brain injury.
Therapy Tip: Record a video of the patient performing an everyday task. While watching the video together, ask them to identify their errors. Be sure to highlight their strengths and suggest strategies they can use next time.
Cicerone et al. (2022) discussed the Pause-Prompt-Praise method for a structured approach to feedback that can be used in different settings:
Once the patient starts building offline and online awareness, it’s helpful to document specific challenges caused by their injury and list individualized strategies they can use during activities of daily living.
Final Thoughts on Awareness
Awareness and metacognition are critical for navigating everyday life, especially for individuals recovering from a brain injury. Impaired awareness can hinder therapy outcomes, but targeted assessments and structured interventions focused on self-monitoring and direct feedback can help individuals regain insight and independence.
Learn More about Awareness
We used many references to bring you this information, all linked where cited. We recommend these selected sources for a good overview:
- Cicerone, K. D., Dams-O’Connor, K., Eberle, R., Fraas, M., Ganci, K., Langenbahn, D., Shapiro-Rosenbaum, A., Tate, R. L., & Trexler, L. E. (2022). The ACRM Cognitive Rehabilitation Manual & Textbook: Translating Evidence-based recommendations into practice. ACRM Publishing.
- Dromer, E., Kheloufi, L., & Azouvi, P. (2021). Impaired self-awareness after traumatic brain injury: A systematic review. part 1: Assessment, clinical aspects and recovery. Annals of Physical and Rehabilitation Medicine, 64(5), 101468.
- Dromer, E., Kheloufi, L., & Azouvi, P. (2021b). Impaired self-awareness after traumatic brain injury: A systematic review. part 2. consequences and predictors of poor self-awareness. Annals of Physical and Rehabilitation Medicine, 64(5), 101542.
- Jeffay, E., Ponsford, J., Harnett, A., Janzen, S., Patsakos, E., Douglas, J., Kennedy, M., Kua, A., Teasell, R., Welch-West, P., Bayley, M., & Green, R. (2023). INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, part III: Executive functions. Journal of Head Trauma Rehabilitation, 38(1), 52–64.
Cite this article: Shahid, S. (2025, June). What SLPs Need to Know: Awareness. Tactus Therapy. https://tactustherapy.com/treating-awareness-after-brain-injury-slp/