What SLPs Need to Know:
Executive Functioning
13 min read
Despite the name, executive functioning isn’t about running a business – it’s more about “adulting.” As we grow up, we learn to set goals and work toward achieving them, monitoring our progress along the way. These could be exciting objectives, such as planning a vacation or getting a new job, but more often they’re routine yet essential tasks, like paying bills, cooking dinner, or managing a busy schedule.
Executive functions (also known as executive or cognitive control) are a set of high-level cognitive skills responsible for monitoring and regulating goal-driven actions. When executive functioning becomes impaired due to a brain injury, day-to-day tasks can quickly become overwhelming and feel impossible to complete. Clinicians, such as speech-language pathologists and occupational therapists, play a crucial role in helping their patients rebuild executive functioning to promote productive and independent lives.

There isn’t a consensus in the literature about which specific skills fall under the umbrella of executive function, probably because they’re all so interconnected. Many studies name inhibition, working memory (specifically updating mental representations), and cognitive flexibility (or shifting) as core functions, as well as the following related skills:
- Reasoning
- Problem-solving
- Planning
- Organization
- Task initiation
- Time management
- Abstract thinking
- Multitasking
If a patient is experiencing new or worsened executive dysfunction, it can seriously impact their ability to achieve meaningful goals in and outside of therapy. In fact, executive functioning predicts clinical outcomes better than attention, processing speed, or memory (Spitz et al., 2012).
Causes of Executive Dysfunction in Adults
Problems with executive functioning can be developmental (starting in childhood) or acquired later in life after normal development has occurred. The scope of this article is limited to acquired executive dysfunction, usually related to injury or a medical condition of the brain.
Stroke (CVA)
It’s been reported that 25-75% of stroke survivors experience executive dysfunction (Sakai et al., 2024). Stroke survivors are more likely to have executive functioning impairments before their stroke compared to healthy adults, and they might experience a cumulative effect post-stroke (Skidmore et al., 2023). This is because executive functioning impairments are associated with brain changes caused by cerebrovascular risk factors and disease, like hypertension and type 2 diabetes. Clinicians should not overlook cognitive deficits in their stroke patients, even if language impairments are more apparent.
We’re working on an article highlighting the overlap between executive function disorders and aphasia. Watch this space for the link later in 2025!
Traumatic Brain Injury (TBI)
Executive functions are associated with the frontal lobes of the brain, a vulnerable area when it comes to traumatic injury (Cisneros et al., 2021). They are also connected with other brain regions commonly affected by TBI, so executive dysfunction is possible even if the frontal lobes are not directly involved. Tsai et al. (2021) reported executive dysfunction in 48% of moderate-severe TBI cases in the subacute phase. In the case of concussion, executive dysfunction has been reported in the acute, intermediate, and chronic stages after injury (Collins et al., 2023).
Looking for Printable Resources?
Unlock the Handout Vault
Dozens of high-quality, well-researched PDF handouts are available all in one place: The Tactus Virtual Rehab Center!
Patient education, home practice, clinical guides, visual supports, & a summary of this article for quick reference.
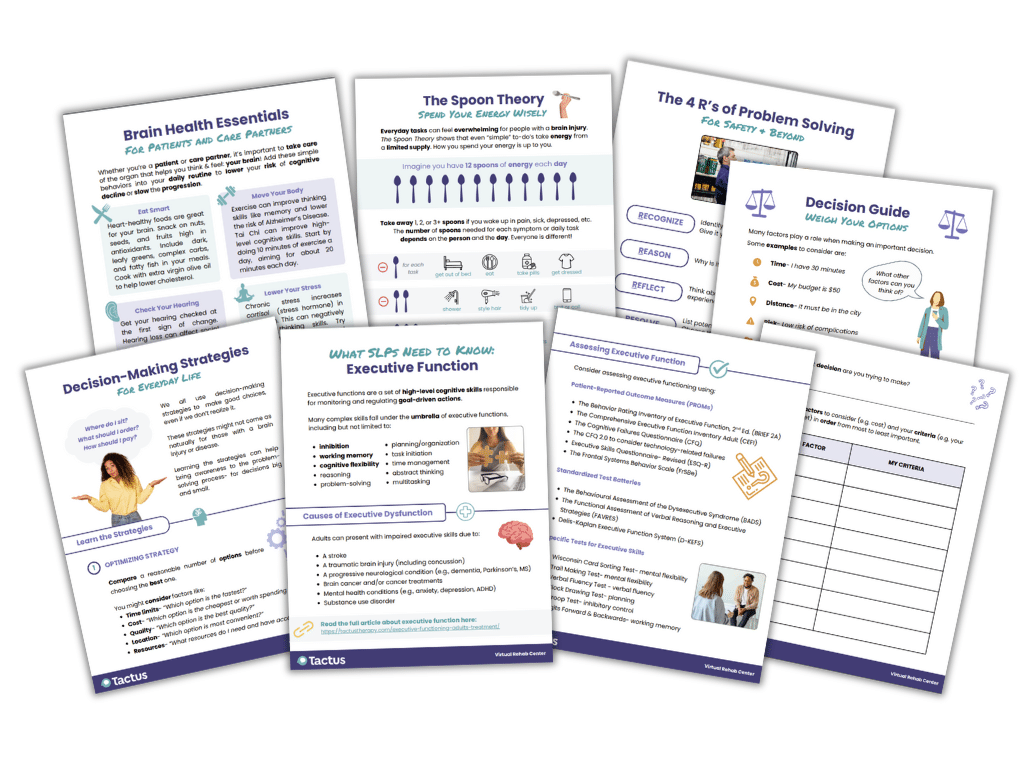
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
Access 50+ evidence-based treatments and 90+ handouts created specifically for adult medical speech-language pathologists.
Neurodegenerative Conditions
Poor executive function is common in progressive neurological diseases and can lead to difficulties with daily living, employment, medication adherence, and social functioning (Duggan et al., 2016). In Alzheimer’s disease, executive deficits may appear early due to changes in the prefrontal cortex (Guarino et al., 2019). Impaired skills may include attention, visuospatial function, and inhibition, but vary depending on the stage of Alzheimer’s disease and the patient’s characteristics. Other dementias, such as frontotemporal dementia, also involve executive dysfunction.
Motor-related conditions like Parkinson’s disease, amyotrophic lateral sclerosis, and multiple sclerosis frequently affect executive skills. Other disorders that may affect the executive system include Huntington’s disease, Creutzfeldt-Jakob disease, progressive supranuclear palsy, and corticobasal degeneration (McCulloch, n.d.).
Brain Cancer
Clinicians might rightfully expect tumors in the frontal lobe to impact executive function; however, tumors in other regions can also result in deficits due to mass effect, swelling, or disrupted subcortical pathways (Loughan et al., 2019). Patients have reported that cancer treatments, such as chemotherapy, have a noticeable impact on cognition. The term “chemo brain” is sometimes used to describe these changes that often impact executive functioning skills.
Other Causes
Executive dysfunction in adults is associated with many mental health conditions, including anxiety, depression, and ADHD. Although people with these conditions might not experience a sudden shift in cognitive skills (like stroke or TBI patients), it’s important for clinicians to be aware of a possible cumulative effect and make appropriate referrals. Duggan et al. (2016) found that executive dysfunction was independently associated with worse severity of depression in intensive care (ICU) survivors, which occurs in 1 of 3 people within the first year post-hospitalization.
Clinicians can use these free screening tools for depression:
Substance use disorder has also been linked to executive dysfunction, given that addiction transitions a person away from goal-directed behavior (executive control) and toward habit-driven behavior (Brockett et al., 2018). The most prominent deficit in people with substance use disorder is inhibitory control, which can unfortunately increase the risk of staying addicted or relapsing (Inozemtseva & Núñez, 2019). Clinicians should be aware of any substance abuse in a patient’s history and recognize the potential impact on cognitive processes.
Assessing Executive Functioning
Since many distinct yet related skills fall under the umbrella of executive functioning, it’s important to conduct a thorough assessment to guide treatment in the right direction.
Patient-reported outcome measures (PROMs) are a good starting point for identifying patients’ unique challenges. These PROMS take 15 minutes or less to administer:
- The Behavior Rating Inventory of Executive Function Second Edition (BRIEF 2A) – $$$
- The Comprehensive Executive Function Inventory Adult (CEFI) – $$
- The Cognitive Failures Questionnaire (CFQ) (PDF) – FREE
- The CFQ 2.0, updated by Goodhew & Edwards (2024) to consider technology-related failures – FREE
- Executive Skills Questionnaire- Revised (ESQ-R) – FREE
- The Frontal Systems Behavior Scale (FrSBe) – $$$
There are also standardized assessment batteries that examine multiple areas of executive function, such as the Behavioural Assessment of the Dysexecutive Syndrome (BADS), the Functional Assessment of Verbal Reasoning and Executive Strategies (FAVRES), or the Delis-Kaplan Executive Function System (D-KEFS). As digital options, the STAC and FSTAC tests are iPad apps that assess cognitive abilities.
Faria et al. (2015) discussed tests that examine specific executive skills, including:
- Wisconsin Card Sorting Test – mental flexibility
- Trail Making Test – mental flexibility
- Verbal Fluency Test (FAS & animals) – verbal fluency
- Clock Drawing Test – planning
- Stroop Test – inhibitory control
- Digits Forward and Backwards – working memory
The Tactus Advanced Naming Therapy app contains the Verbal Fluency Test for F,A,S and animals with norms in the report.
It’s important to observe the patient during the assessment period to gain insight into their executive skills. Notice if they are retaining directions, detecting and correcting errors, staying on task, or needing extra assistance. Also note any factors that might interrupt goal-directed behavior, such as frustration or defensiveness.
Overall, these cognitive assessments will help identify patients’ strengths and weaknesses, guiding clinical decision-making and goal setting. With a better understanding of the challenges, clinicians can move forward with targeted treatment approaches to support their patients.
Treating Executive Dysfunction
Metacognitive strategy instruction (MSI) is one of the most widely used evidence-based approaches in cognitive rehabilitation. Most metacognitive protocols for executive functioning include self-monitoring, feedback, and emotional regulation components, and they’re often combined with other approaches, such as external aid training (Jeffay et al., 2023; Sohlberg et al., 2023). Clinicians use education, modeling, directions, handouts, and cuing to help patients internalize and use strategies more automatically during everyday tasks (Cicerone et al., 2022).
The Role of Awareness
Effective MSI requires some level of self-awareness to know when and how to use strategies in the real world (although MSI itself improves awareness). If self-awareness is impaired, clinicians should address it first using evidence-based techniques, like Awareness Training or Pause-Prompt-Praise.
Learn how to assess and treat awareness by reading What SLPs Need to Know: Awareness
Once the patient can recognize their challenges, the clinician can choose a metacognitive approach to target executive skills. The goal of MSI is for the patient to work toward a meaningful goal while regulating their thoughts and behaviors. The clinician should teach the strategy in the context of tasks that are both functional and relevant for the individual.
A Focus on Self-Monitoring
One effective strategy is verbal mediation, also known as self-talk. In this approach, patients are taught to say the steps of a task out loud as they complete it, then gradually reduce the volume to a whisper, and eventually to internal speech. This technique can help individuals stay focused and catch errors in real-time.
Another helpful strategy is the WSTC acronym (Sohlberg et al., 2023) to guide patients through the self-monitoring process:
- What am I supposed to be doing?
- Select a strategy (e.g., an external aid, emotional regulation, or memory support).
- Try the strategy.
- Check that the strategy worked.
Problem-Solving Treatments
Problem-solving approaches are another option to rehabilitate executive function. Clinicians can use Short-Term Executive Plus (STEP), a treatment that involves problem-solving, emotional regulation, attention, and the use of cognitive supports (e.g., using a calendar or to-do lists) (Cantor et al., 2014). STEP involves direct instruction in both individual and group formats.
STEP uses a 5-step SWAPS approach:
- Stop! Is there a problem?
- What is the problem?
- Alternatives and options to solve the problem
- Pick and plan the chosen option
- Satisfied with the outcome of the plan
During the emotional regulation portion of STEP, participants learn about the relationship between thoughts, emotions, and behaviors. They also learn skills to help regulate emotions through classroom instruction and repeated practice. Patients can learn to identify their emotional triggers, name their emotions, reframe negative thoughts, and practice mindfulness to help them regain emotional control after injury (McGarvie, 2025).
Put SWAPS into Action
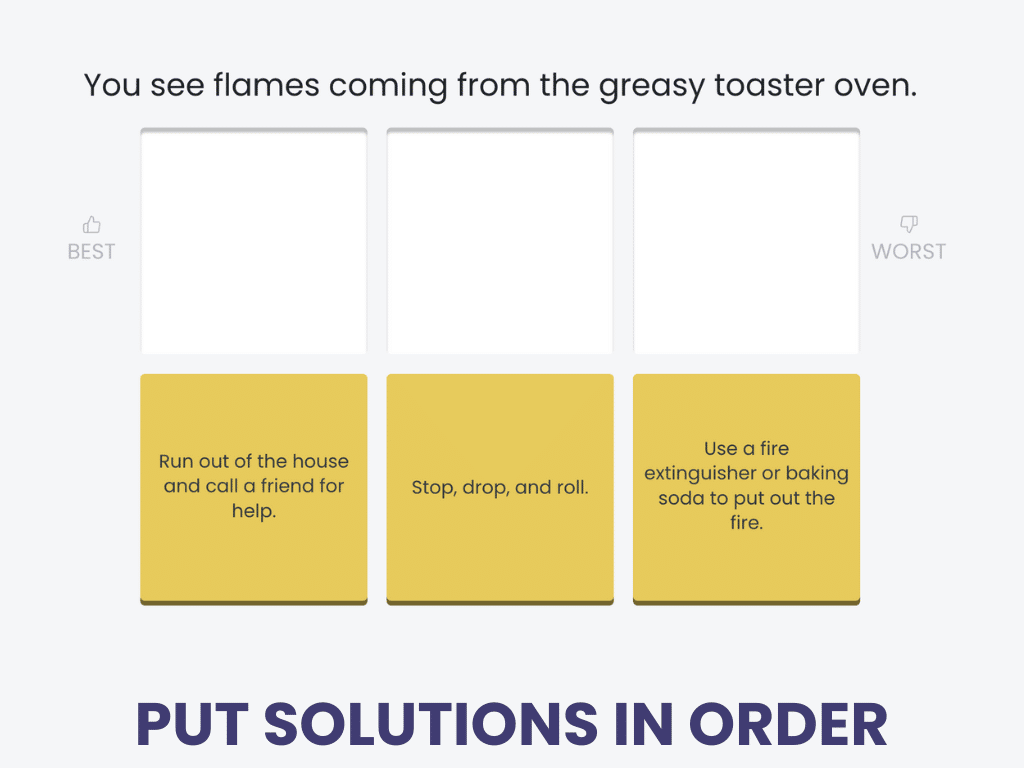
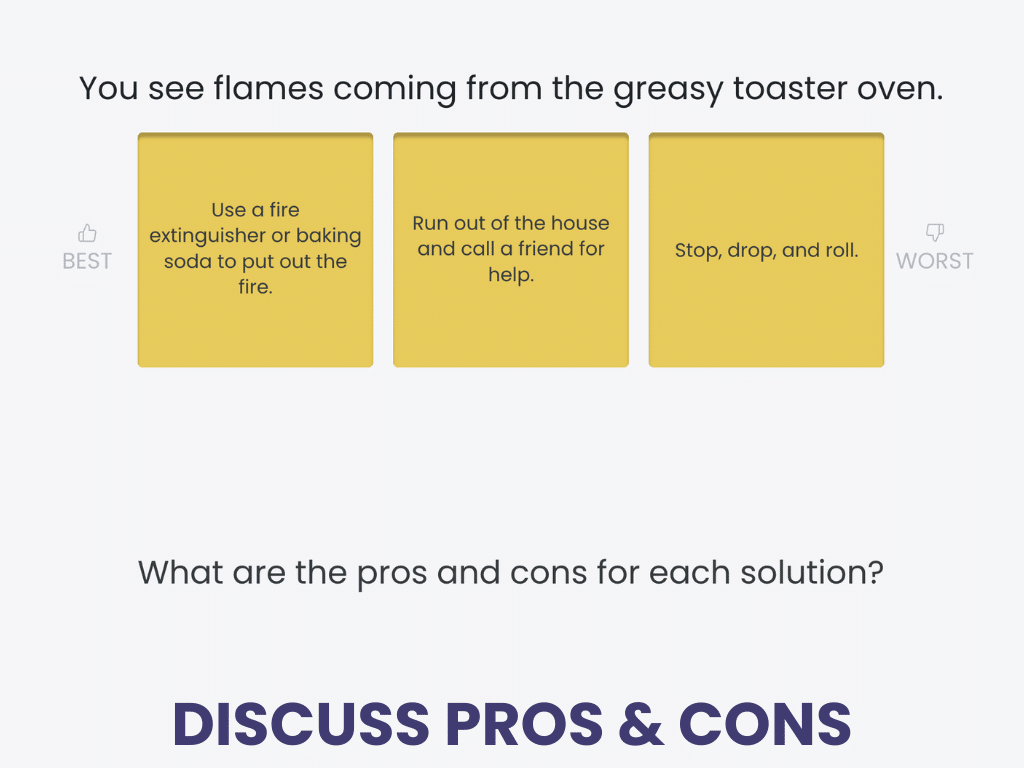
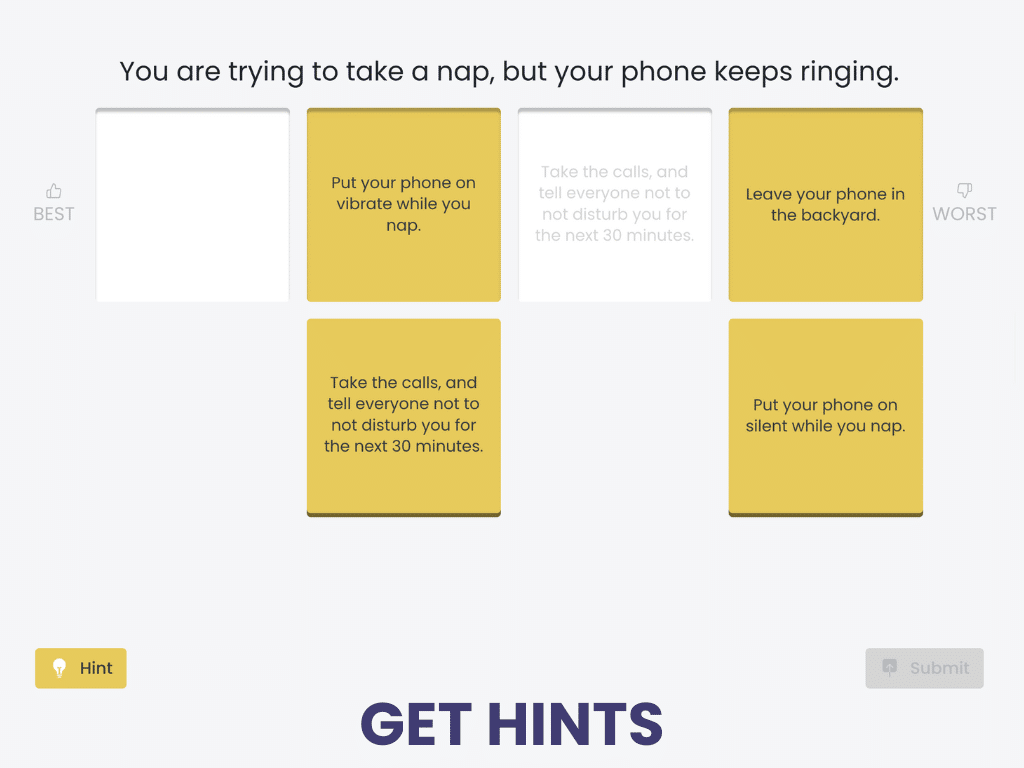
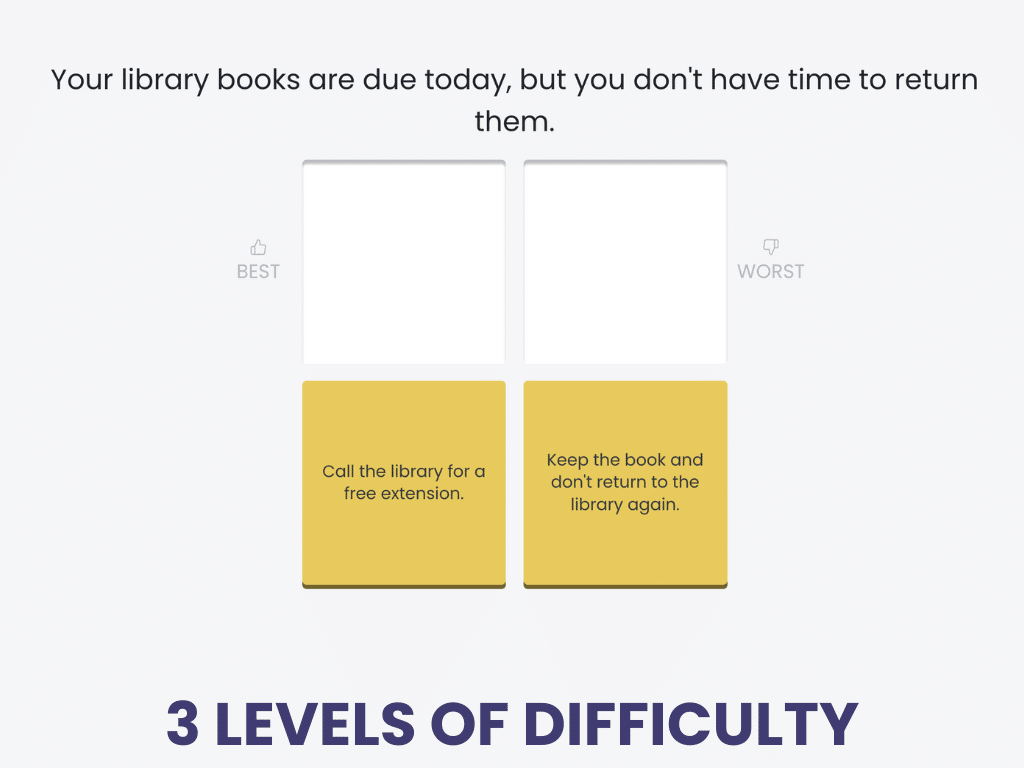
Ranking Solutions to Problems
Ranking Solutions to Problems is a cognitive treatment for executive functioning in the Tactus Virtual Rehab Center.
Patients read a problem, then place 2-4 options in order from best to worst. They’re prompted to discuss the pros and cons of each option.
Ranking Solutions to Problems is based on the SWAPS approach to problem-solving. A non-verbal problem-solving treatment is also available, called Solving Pictured Problems.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
Goal-Driven Treatments
There are several goal-focused therapy protocols that have a lot of features in common:
All these approaches are complex, so patients with more severe conditions will need significant scaffolding and cueing. If the procedures are still too challenging, clinicians can present them in an errorless learning format when possible.
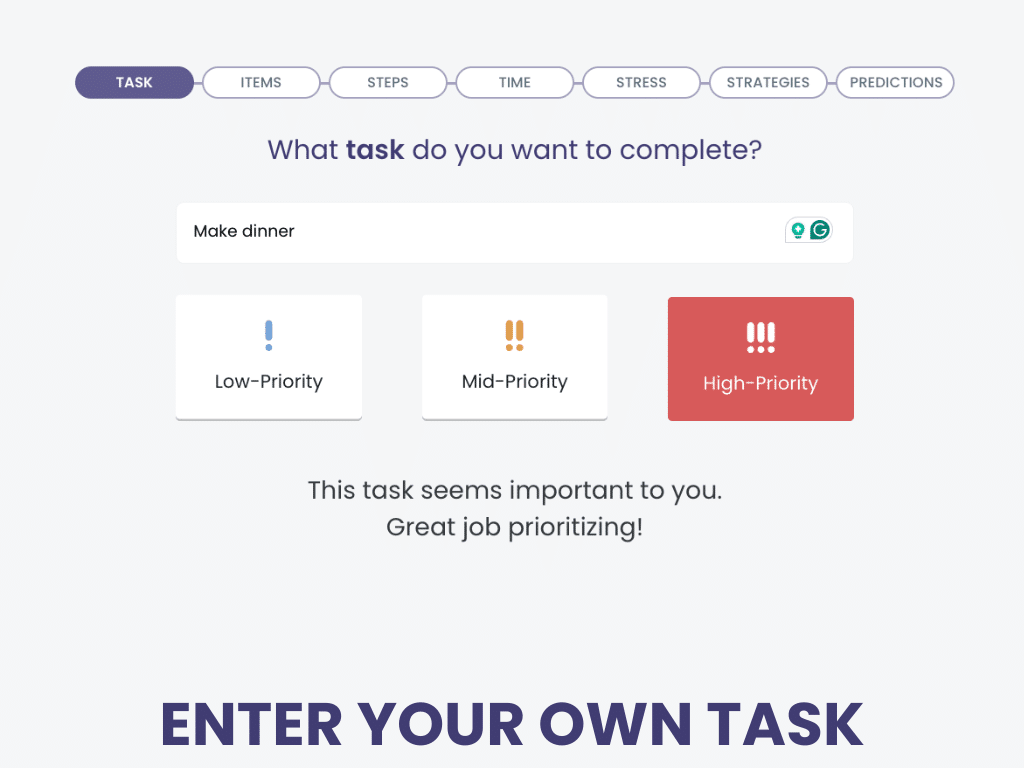
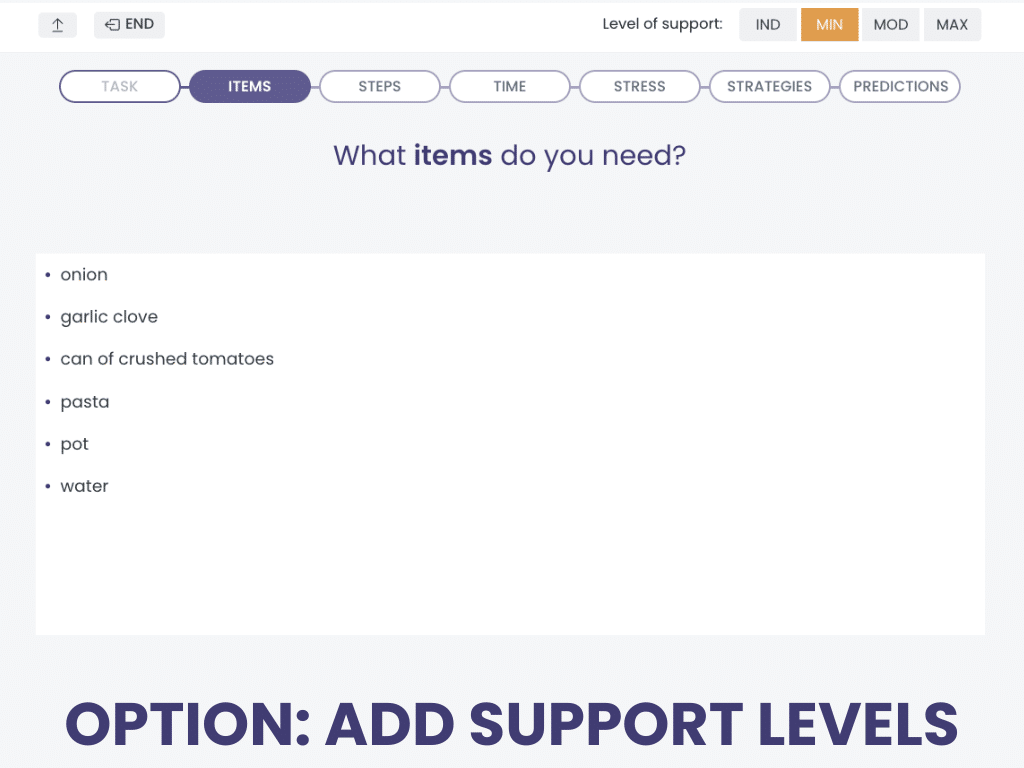
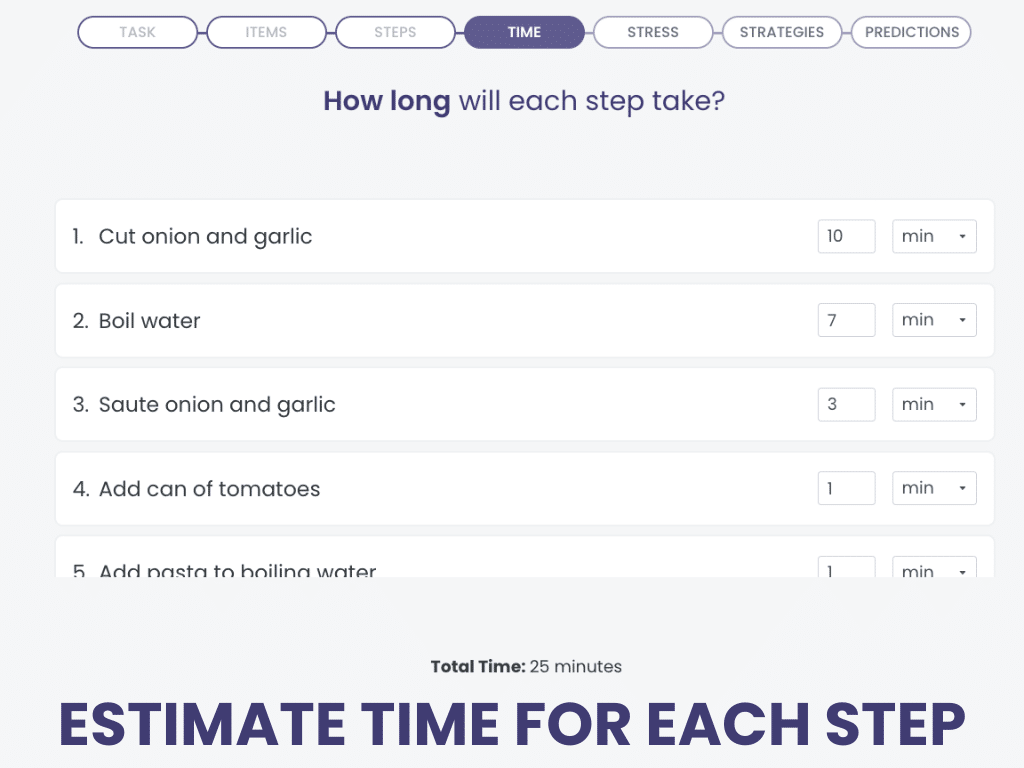
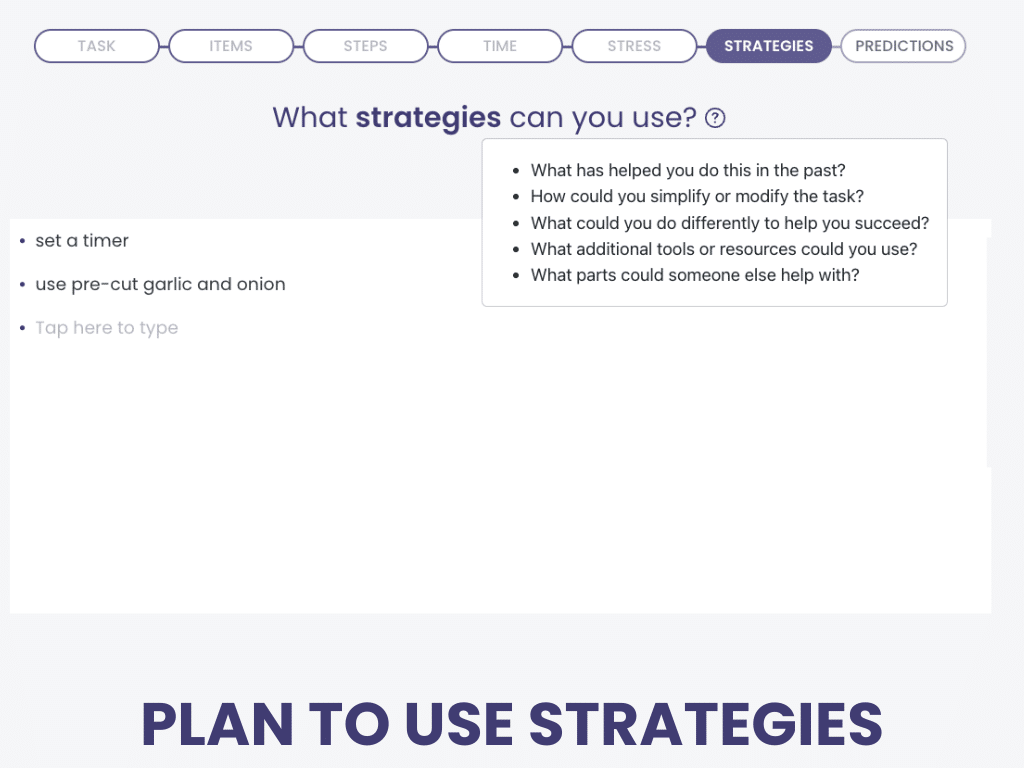
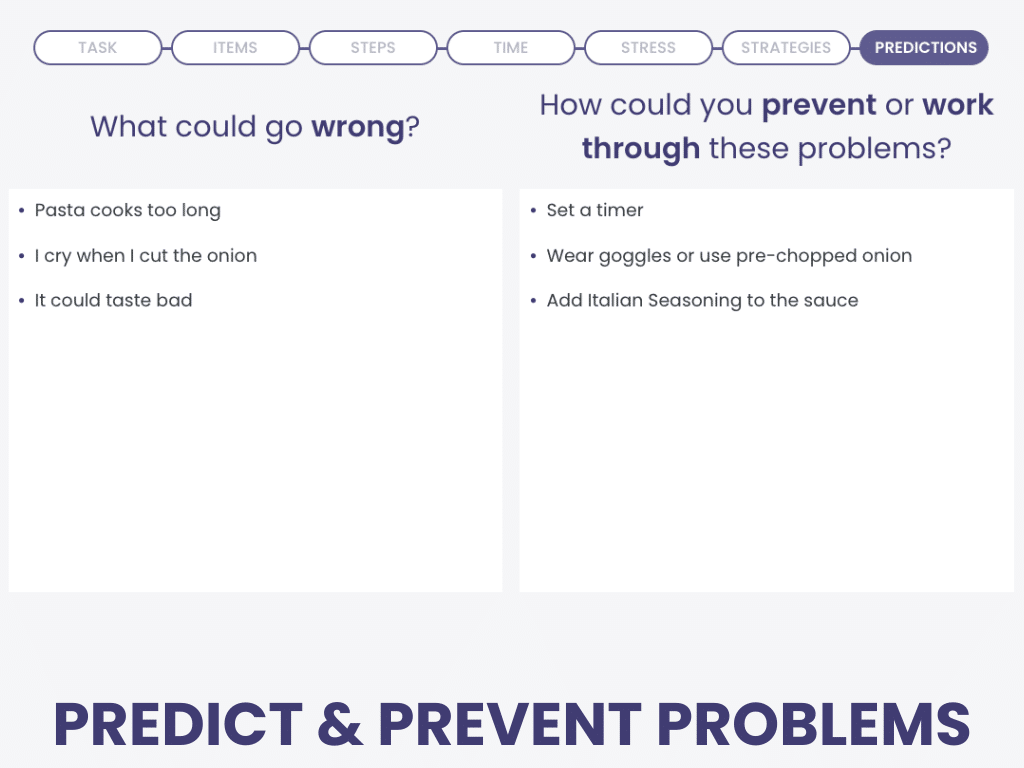
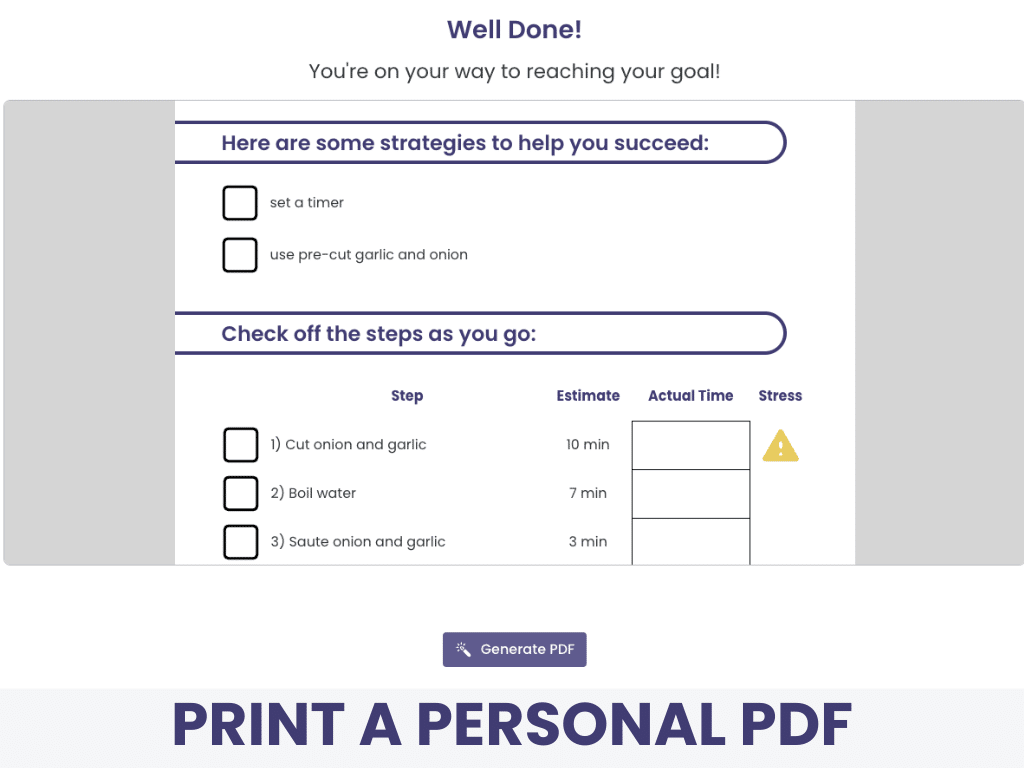
Put Goal-Plan-Do-Review to Work:
Planning Your Tasks
Planning Your Tasks is a cognitive treatment in the Virtual Rehab Center that helps patients with executive functioning impairments.
Work through planning, executing, and reflecting on a personally meaningful task, step by step, in our 7-part sequence that includes all the core elements of MST.
Planning Your Tasks provides a printable PDF at the end of the treatment to facilitate follow-up after the task has been completed.
Sign up today for a risk-free 21-day trial of this innovative web-based therapy platform for SLPs.
If your patient isn’t ready to work on a personal goal, practice the steps using the simplified Planning Tasks treatment with choices!
Beyond Traditional Treatments for EF
Although metacognitive strategy instruction is the gold standard for addressing executive dysfunction, there are some innovative approaches that clinicians can consider. These creative methods engage the brain in unique ways and can have a positive impact on daily functioning.
Virtual reality can be used to supplement in-person therapy for patients with TBI (Jeffay et al., 2023). Clinicians might think virtual reality is limited to a fully immersive experience using a headset, but it can also be non-immersive, involving just a keyboard and screen. It isn’t limited to one specific approach either; it can be game-based, task-oriented, or simulate instrumental activities of daily living.
Tech Tip: Mobile apps can provide real-time help with task management outside of a clinical setting. Tools like Focus Keeper and Todoist offer structure through timers, checklists, and reminders, making it easier for patients to stay organized and follow through with strategies independently.
Dance therapy has been found to positively impact executive function skills in patients with Parkinson’s disease (Zhang et al., 2019). It combines physical and cognitive movements in an enjoyable and creative space, which makes adherence more likely compared to other programs.
Music therapy can be used to address executive dysfunction, even if the patient (or clinician) doesn’t have musical experience. Siponkoski et al. (2020) describe three components of a program: rhythmic training, cognitive-motor training, and assisted music playing. Research has found improvements in general executive functioning (including self-monitoring and set-shifting skills) and brain changes following music therapy (Jeffay et al., 2023).
Final Thoughts on Executive Functioning
Executive dysfunction can have a profound impact on everyday life for individuals recovering from brain injury or managing a progressive neurological condition. The good news is that there are evidence-based, functional treatment approaches that clinicians can implement to make a real difference.
By understanding the underlying causes, selecting the right assessments, and using metacognitive strategy training (or other creative methods), clinicians can help patients regain control. Treating executive function is not just possible —it’s essential to helping patients rebuild their independence and quality of life.
Learn More about Executive Functions
We used multiple references to provide you with this information, all of which are linked where cited. We recommend these selected sources for a good overview:
Cite this article: Shahid, S. (2025, July). What SLPs Need to Know: Executive Functioning. Tactus Therapy. https://tactustherapy.com/executive-functioning-adults-treatment/