5 Things People Don’t Understand about AAC for Aphasia
7 min read
Many people have the misunderstanding that “AAC” is an expensive app or a specialized speech-generating device. In fact, there is no one thing that is AAC. AAC (augmentative and alternative communication) is actually anything that can supplement or replace communication for a person whose own communication is insufficient or ineffective. It can be strategies, techniques, or devices. It can be no-tech, low-tech, or high-tech. It can be used independently or aided by a communication partner.

Here are 5 other common misconceptions about AAC, especially as it relates to aphasia:
1) AAC is not a magic cure for aphasia.
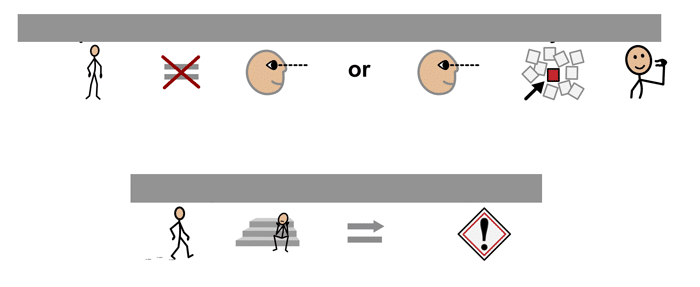
Aphasia is not like losing your voice – the words are not going to pour out in the correct order if you can only find the right app. Aphasia affects symbolic communication of all types; both grammar and syntax are impaired, as well as understanding of icons that symbolize concepts. Many people with severe aphasia struggle to match a drawing of a cup with a real cup. How can we then expect them to use a tool that requires matching a picture of a cup with their feeling of thirst?
Putting an AAC tool in the hands of a person with aphasia will probably not enable them to immediately start expressing themselves. They need personalized, contextualized communication supports that adapt to their evolving needs. They need to be trained to use their tools, and not just once.
2) Most AAC tools were not created with aphasia in mind.
Clearly Stephen Hawking’s speech-generating device would not be appropriate for someone with aphasia. Most text-based AAC apps and devices are designed for people with intact language but limited speech – people with conditions like laryngitis, Autism, cerebral palsy, ALS, or head and neck cancer. This leads therapists or families toward symbol-supported communication apps for people with aphasia.
The problem with the popular grid-based app is that it requires a great knowledge of the words you want to include in your message. For example, to construct “Let’s go to the store”, you must know that “Let” is a verb, but consider whether “Let’s go” is stored in the Quick Phrases folder. You also need the memory to hold onto the full message (after “to” you want to say “the”), in addition to visual attention and executive functioning to navigate screens full of folders and icons. If reading is impaired, the user must rely on symbols, and those symbols aren’t always transparent.
There are a small number of apps and devices made with aphasia in mind. Designed by SLPs or linguists and tested on stroke populations, these apps use evidence-based theories of what works with aphasia (e.g. visual scene displays, navigation rings, personalization, stored messages). But even these tools can be limited in their usefulness, helping to communicate predictable things, but often unable to adapt to an evolving conversation.
3) One size never fits all (or won’t fit for long).
Buying AAC apps for a person with aphasia can be like buyings shoes for a child in a growth spurt: necessary, but only useful for a short period of time. Many people with aphasia are working hard to recover their ability to communicate; a customized AAC tool will hopefully be made irrelevant through therapy and continued practice. And about that customization – someone has to spend the time, perhaps repeatedly, to adapt the tool to the user.
For people with aphasia, often the most effective AAC is provided through a system of tools and strategies. Like using the Maps app to show where you live, switching to Contacts to find a name, and using a pocket notebook to reference words or draw pictures. Switching tools, to the one that provides just the right information, requires strong cognitive skills and may take some training. But it’s a therapist’s goal is to encourage independence and improve quality of life – teaching to fish rather than giving a fish.
AlphaTopics AAC is a flexible tool for people with aphasia to use when communication breaks down. It includes a white board, a topic board, and a letter board that can be quickly referenced, easily customized, and kept handy on a phone or tablet.
AlphaTopics AAC
Enhance & clarify natural speech with this simple yet powerful augmentative communication app for dysarthria & aphasia.
4) AAC is not a one-way street.
Learning to use an AAC system can be like trying to learn a new language, for both communication partners. You cannot simply put an app or device into someone’s hands and expect them to easily turn their ideas into words, or to even want to. A person with aphasia will need to see how it can be used to express a variety of concepts, and to see that it’s acceptable to communicate in this way. They need to see you use it.
Modelling how to use the system not only teaches the person with aphasia, it can also be an invaluable learning experience for the clinician or family member. You’ll begin to see how difficult it is to find the right message, or if that message is there at all. You’re bound to develop more empathy as you see how using AAC slows the conversation, requires much more effort, and forces you to mentally edit your message accordingly.
Aided language input is an evidence-based intervention that is motivating and can help people learn to use AAC faster.
Use of augmentative tools by people without aphasia is also an effective way to make sure you’re getting your message in. By writing down keywords, drawing, and using pictures as you talk, you’re making it easier for the person with aphasia to understand what you’re saying. Once your message goes in, then the tools are all in place to help them get their message out.
5) AAC is not the last step in aphasia therapy.
You cannot just wait until the end of a person’s time in therapy to send them home with an app or device. Issues with finding, funding, and personalizing an AAC system guarantee that almost no therapist will be able to equip a client quickly. Those same issues require that a therapist begin introducing AAC as soon as they identify that such an approach would be beneficial. Fortunately, there are free AAC assessment tools to help therapists assess the needs and abilities of people with aphasia to facilitate the feature-matching process.
There’s a persistent misconception that AAC is a last-ditch effort once therapy fails: “once the person hits a plateau, meaning they’re never going to improve and therapy isn’t worthwhile, it’s time to try AAC.” Not one bit of that is true. Nobody with aphasia is ever without hope of improving, virtually nobody will fail to benefit from therapy, and AAC should not be regarded as only helpful once therapy is exhausted.
If AAC tools are introduced early in the therapeutic process, alongside restorative techniques, they are more likely to be accepted, used, and useful in supporting communication. There will be more time to demonstrate their use, customize them, and train family members to use them outside therapy. AAC provided on the way out the door is almost guaranteed to end up covered in dust or never used.
A Better Understanding of AAC and Aphasia
It’s no wonder that so many people with aphasia reject efforts to provide them with an AAC system. They know that most apps have too many icons, words, or screens for them to make sense of. They know they’re being asked to communicate differently. They know the system can’t say everything they want to say. They know when it’s a last resort.
So as therapists, we need to do better. We need to know which tools are effective for people with aphasia. We need to introduce them early and often. We need to properly assess, match, train, model, and adapt. All of this will help people with aphasia participate better in their lives, it will reveal their competence and intelligence, and it will make our efforts more effective.
Resources for AAC and Aphasia
For more information about the latest developments in AAC and aphasia, check out Dr. Sarah Wallace’s course on SpeechPathology.com. For a comprehensive look at communication supports in aphasia, this textbook is an excellent resource. If you missed the link to it above, be sure to check out the Aphasia Assessment Materials from Drs. Garret and Lasker, as well as their extremely helpful ASHA Leader article.
Want to make your own custom communication boards for FREE? Discover this AAC hack with video instructions from our newsletter!
If you’re wondering what the icons above say, it’s: “This person cannot see or sees only a little. Walking alone could be dangerous.” Didn’t the symbols make it clear?
