27 Dysphagia Myths – Busted!
12 min read
Swallowing disorders are serious business, and the speech-language pathologists who assess and treat them need to know their stuff. Unfortunately, there are many dysphagia myths floating around out there, and SLPs are constantly having to educate patients, families, and other medical staff to combat these contagious pieces of misinformation. Here are some they want you to stop believing:
Sometimes A Cough is Just a Cough
1) Myth: If you don’t cough, you aren’t aspirating.
2) Myth: If you cough, you’re aspirating.
Truth: A cough is a protective reflex meant to expel things from the airway. A strong cough is a good sign you’re actually not getting food caught in your lungs. A cough can be a sign of aspiration, but it can also be the way a person protects themselves from aspiration. It can also be from another medical condition and completely unrelated to eating. But as above, you need to actually see what’s happening to know for sure.
3) Myth: If you cough, you’re choking.
Truth: Related to the one above, coughing is protective. It takes air to cough, so if you’re coughing, you’re breathing. Technically, choking is about not being able to breathe because something is obstructing the airway, but the term “choking” is often confused with “coughing”. Please be specific when documenting trouble at mealtimes. Was the person coughing or choking? If he was choking, you should probably give the Heimlich maneuver instead of writing it down.
Download the handout to share with staff!
Get your free 2-page PDF handout of 16 Dysphagia Myths – Busted! We’ve summarized over half of these myths for you in an easy-to-read handout that is perfect for inservices or staff education.
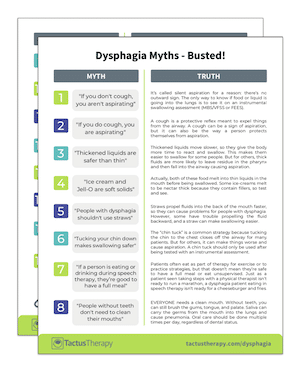
In addition to receiving your free download, you will also be added to our mailing list. You can unsubscribe at any time. Please make sure you read our Privacy Policy and Terms & Conditions.
Thickened Liquids
4) Myth: Thickened liquids are safer than thin.
Truth: Thickened liquids move slower, so they give the body more time to react and swallow. This makes them easier to swallow for some people with dysphagia. But for others, thick fluids are more likely to leave residue in the pharynx and then fall into the airway, and they are harder to clear. Patients are also less inclined to drink fluids the thicker they are, so a recommendation for honey-thick fluids may result in dehydration, which can cause a multitude of other health issues.

5) Myth: Thickened liquids must be recommended along with modified solids.
Truth: Food and liquid recommendations are not dependent on one another. It’s possible to be safest on thin liquids and pureed solids (if the oral phase is weakest), or on regular solids with thickened fluids. SLPs do a detailed assessment that looks at the underlying impairments, and food/drink recommendations are made separately, based on those findings. Don’t assume that a “dysphagia diet” is pureed food with honey-thick fluids.
6) Myth: If a person is on thickened liquids, they can never have water.
Truth: Water is sometimes recommended as the only thin liquid a person can have if good oral care can be ensured. The Frazier Free Water Protocol is a procedure of offering water for some dysphagia patients to keep hydration up – especially those who are otherwise medically stable and physically active. The idea is that even if a small amount of pure water is taken into the lungs, the body will clear it without infection. That’s why good oral care is essential.
Modified Solids
7) Myth: People without teeth can’t eat a regular-texture diet.
Truth: Some people have strong gums and can actually bite into a raw apple. Don’t assume what a person can eat based on their dentition. Ask and observe.
8) Myth: Ice cream and Jell-O are soft solids.
Truth: Actually, both of these food melt into thin liquids in the mouth before being swallowed. If a person is not safe with thin fluids, they are likely not safe with these items either. Some ice-creams melt to be nectar thick because they contain fillers, so test and see.
9) Myth: If a person can have thin liquids and soft solids, they’re good to have Minestrone soup.
Truth: Dysphagia diets often restrict “mixed textures.” These are foods that combine two or more textures together, like non-blended soups, cereal with milk, and even juicy fruit like grapes or oranges. Mixed textures are harder to control in the mouth. If the patient has difficulty with mixed textures, soups should be blended or simply broth, and cereal should absorb the milk or be drained.

10) Myth: Cooked rice and corn are part of a dysphagia diet because they are soft.
Truth: Maybe. These are tricky foods that don’t form a cohesive bolus in the mouth. Grains like rice, corn, and barley scatter in the mouth. There are some preparations that may lessen the risk (like risotto or congee for rice), but it’s important to test the individual food.
Dysphagia diets can be confusing! Isn’t there a standard? Why yes, now there is! The International Dysphagia Diet Standardisation Initiative, or IDDSI, has developed global standardised terminology and definitions for texture modified foods and thickened liquids to improve the safety and care for individuals with dysphagia. Check out their tests to see what texture a food or liquid really is!
Swallowing Strategies
11) Myth: People with dysphagia shouldn’t use straws.
Truth: Straws propel fluids into the back of the mouth faster, so they sometimes cause problems for people with dysphagia. However, some people have trouble propelling the fluid backward, and a straw can make swallowing easier. It’s always best to test what effect a straw makes during an instrumental assessment to know for sure.

12) Myth: Tucking your chin down makes swallowing safer.
Truth: The “chin tuck” is a popular compensatory strategy for swallowing impairments. Tucking the chin to the chest closes off the airway for many patients, but for others, it can make things worse and actually cause aspiration. Use of a chin-tuck strategy should always be tested with an instrumental assessment to see what impact it has on the swallow.
13) Myth: Smaller bites are always safer than big ones.
Truth: For people with reduced sensation, a bigger bite may give more sensory information and can be swallowed more safely. It’s important to test bolus size on instrumental assessments to know what size is best.
14) Myth: If a person is eating or drinking during speech therapy sessions, they’re good to have a full meal, sips of water, or their favorite snacks.
Truth: Patients often eat as part of therapy for exercise or to practice strategies, but that doesn’t mean they’re safe to have a full meal or eat unsupervised. Just as a patient seen taking steps with a physical therapist isn’t ready to run a marathon, a dysphagia patient eating in speech therapy isn’t ready for a cheeseburger and fries.
Bring the Dysphagia Therapy app with you into the assessment to quickly get a list of the strategies you can try before the assessment ends. Enter your assessment findings (impairments and observations) into the Therapy Finder for an instant list of evidence-based treatments to consider.
Oral Care for Dysphagia
15) Myth: People without teeth don’t need to clean their mouths.
Truth: EVERYONE needs a clean mouth. Without teeth, you can still brush the gums, tongue, and palate. Saliva can carry the germs from the mouth into the lungs and cause pneumonia, and we sometimes aspirate a little saliva while we sleep, making oral care before bed even more important.

16) Myth: Swabbing the mouth with an oral care sponge is just as good as a toothbrush.
Truth: Toothbrushes and toothpaste are the most effective means of cleaning the mouth. That’s why we all use them at home on ourselves. Good oral care is important for preventing pneumonia, so advocate for your facility to provide toothbrushes and implement oral care guidelines.
Check out this excellent 4 part series from SwallowStudy.com about oral care, why it’s important (spoiler: it prevents pneumonia), and how to do it properly.
Only Diamonds are Forever
17) Myth: The recommendations of the SLP for a specified diet are forever.
Truth: Diet recommendations are put in place to compensate for a swallowing problem while rehab is in progress, so they should regularly change. In the cases of degenerative conditions, diets may be downgraded. If a patient is on a modified diet and isn’t happy or seems to be struggling, ask for a re-assessment.

18) Myth: If someone aspirates during an instrumental swallow study, they shouldn’t eat an oral diet – ever.
Truth: While instrumental assessments are the gold standard, they are only a snapshot in time. Putting a sick person in an unfamiliar room with a large fluoro machine and feeding them barium-coated crackers does not replicate a normal mealtime environment. While FEES can be done in a more natural environment than an MBS/VFSS, eating with a camera tube up your nose is not the normal way of eating either. The study should be repeated after a course of rehab and recommendations adjusted.
19) Myth: If you opt to have a feeding tube, you will never eat again.
Truth: A feeding tube surgically implanted in the stomach can be a good way to get the nutrition you need while your swallow improves. The procedure is reversible, so once you’re getting enough nutrition by mouth, the tube can come out. It’s like a crutch for a sprained ankle – it helps until the problem is healed.
Speaking of Tubes
20) Myth: If you have a feeding tube, you can’t also eat by mouth.
Truth: Related to the myth above, this one is more for the healthcare professionals out there who may try to stop a patient from eating if they’re on a tube. Patients recovering from dysphagia may start to eat a small amount, first therapeutically, then for nutrition. It’s important to involve the dietitian as there may be a need for calorie counts and to adjust the amount of tube feed formula used to prevent unnecessary weight gain.
21) Myth: People with feeding tubes can’t aspirate because they aren’t eating.
Truth: Saliva can be aspirated, as can regurgitated tube feeding liquid and other stomach contents. Feeding tubes are not a fail-safe way to prevent aspiration pneumonia. In fact, tube feed formula sometimes causes acid reflux, and acid in the lungs is particularly dangerous. When dealing with an end-of-life situation, families often opt for a feeding tube, thinking it will help. However, it often only prolongs the inevitable with a painful surgery and removes one of the person’s last remaining pleasures – eating. Consider feeding tubes carefully as there are many pros and cons associated with them. In cases of feeding tubes in patients with advanced dementia, research tells us that the feeding tubes don’t even help most people live longer.
22) Myth: People with trach tubes with an inflated cuff can’t aspirate.
Truth: A cuffed trach might prevent large chunks of food from falling directly into the lungs, just as long as it’s inflated. As soon as it’s deflated, anything sitting on top of the cuff falls right down into the lungs. But more likely, the food particles, liquids, and pathogen-infected saliva are already seeping down around that cuff. Over-inflating the cuff to feel like it’s more protective against aspiration won’t work, since the trachea isn’t a perfect circle. What will work? Better oral care has been shown to reduce pneumonia in ventilated patients.
Signs and Symptoms of Dysphagia
23) Myth: A runny nose while eating is a sure sign of aspiration.
Truth: While a person who is aspirating may have a runny nose, watery eyes, and cough, the presence of only a runny nose while eating is not a predictor of dysphagia. It’s called gustatory rhinitis, and it’s completely normal, especially while eating hot and/or spicy food.
24) Myth: If a person has a diminished gag reflex, they likely have a swallowing disorder.
Truth: Too many doctors are going around sticking tongue depressors down people’s throats in an attempt to determine the presence or absence of a gag reflex for no good reason. While the gag reflex is controlled by cranial nerve IX, an absent gag is a completely normal thing for 37% percent of the population. An overactive gag is also normal, and you could find yourself covered in vomit. Gag is not a reliable predictor of dysphagia, so carefully consider why you’re testing it.
25) Myth: A swallowing test is pass/fail.
Truth: A proper assessment of swallowing is meant to determine what is happening during the swallow and why. Nobody can “pass” or “fail” a swallowing test any more than they can “pass” or “fail” a CT scan. Usually what people mean when they ask for the result is whether or not someone can eat by mouth or have a diet upgrade. Make the SLP’s day by asking what the key findings of the test were and what her recommendations are.

26) Myth: An instrumental study is done solely to determine if a person is aspirating.
Truth: While aspiration can be visualized during instrumental studies, it is not the only reason we test. Even more valuable than seeing aspiration is seeing WHY the aspiration is happening. So even if a patient aspirates on a study, the study might continue to better understand what the physical swallow deficits are.
27) Myth: A good SLP can tell exactly what’s happening through a bedside exam and doesn’t need to do an instrumental assessment.
Truth: We can’t treat what we can’t see, and nobody has x-ray vision. An experienced SLP can tell if someone is really struggling at bedside, or if they’re having difficulty with the oral phase of the swallow. But they can’t see if the airway is protected or look at how the bolus is moving in the throat. They can’t accurately determine the effectiveness of strategies, positioning, or maneuvers.
Thank you to the members of Medical SLP Forum Facebook group for sharing the most common myths they have to bust on a daily basis!