How To:
Treat Wernicke’s Aphasia
10 min read
There are a lot of speech pathologists out there seeking advice on how to treat Wernicke’s aphasia (aka fluent aphasia, jargon aphasia, or receptive aphasia). It’s no wonder when you look at the statistics:
Wernicke’s aphasia occurs in about 15-20% of people with acute aphasia, but a year after the stroke, only 5% of people still living with aphasia have the Wernicke’s type.1
This means that each clinician who treats aphasia will likely see someone with Wernicke’s aphasia at some point, but certainly not every day. People living with Wernicke’s aphasia are even less common in community aphasia groups, where they comprise 1 in 20 people with chronic aphasia.

And each person with Wernicke’s aphasia is also quite different. While all people with this classification have speech filled with nonword jargon with near-normal prosody, there is a good deal of variability in the amount of auditory and reading comprehension that is retained.2
What’s more is that those who have Wernicke’s aphasia seem fairly resistant to treatment. This is not surprising, given that anosognosia, or a failure to recognize one’s impairments, is a common feature. Why would someone want to attend speech therapy or work on improving when they are unaware that they have a communication problem?
But all hope is not lost. Most people with Wernicke’s aphasia recover rapidly.3 For those who don’t, there are some treatments with good results for clients and partners who are motivated to work on improving communication.
What are some treatments for Wernicke’s Aphasia?
There are two published treatment approaches specific to Wernicke’s aphasia that give us a good place to start. While neither has much research evidence to support its efficacy, the treatments are clinically useful and anecdotal reports are extremely positive.
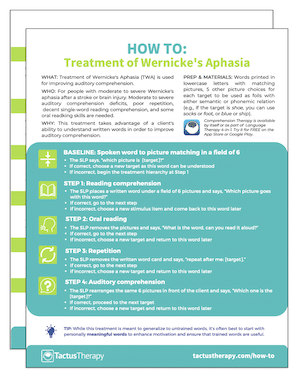
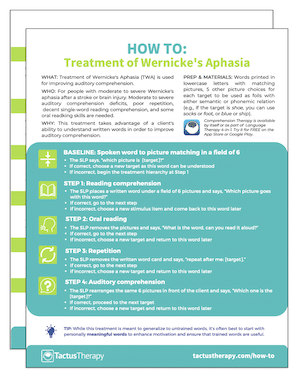
Download a “How To” guide now!
Get your free PDF handout of How To Do Treatment of Wernicke’s Aphasia (TWA). Includes step-by-step instructions and a printable data sheet to use in therapy!
In addition to receiving your free download, you will also be added to our mailing list. You can unsubscribe at any time. Please make sure you read our Privacy Policy and Terms & Conditions.
Speech therapy protocols tested on people with Wernicke’s Aphasia
The volume of research performed on treatments for Wernicke’s aphasia pales in comparison to that for non-fluent aphasia. It consists largely of case studies, with some larger experimental studies that separate out the data for fluent subjects.
Verb Network Strengthening Treatment (VNeST)
Some of the initial research studies for VNeST included subjects with fluent aphasia, including one with moderate-severe Wernicke’s aphasia and one with moderate jargon aphasia, showing improvements. 4 The person must understand well enough to follow the treatment procedure, and written response adaptations can be used.
A case study 5 looking at outcome measurement saw one man with Wernicke’s aphasia receive 24 hours of VNeST over 6 weeks, training 20 verbs 2-3 times each. The participant improved at the treatment task, and while his auditory comprehension skills did not improve, he required fewer repetitions of the audio to get the same accuracy post-treatment. Likewise, scores on tests of verbal expression did not improve, but responses were noted to have fewer non-words for action naming. In an analysis of discourse, the participant had fewer total verbal units (this is a good thing in fluent aphasia) and more relevant content units, and the number of relevant utterances improved by over 10% to 51%. Subjectively, the research participant’s wife noted improved communication with friends. This study highlights the need to expand outcome measures beyond test scores for word- and sentence-level tasks when looking at Wernicke’s aphasia.
Attentive Reading and Constrained Summarization (ARCS)
A study 6 looking at two people with Wernicke’s aphasia, one moderate and one severe, used Attentive Reading and Constrained Summarization therapy to attempt to improve word retrieval. After 18 sessions, the person with moderate Wernicke’s aphasia improved significantly on the Boston Naming Test, a picture description task, and retelling an article; the one with severe Wernicke’s aphasia did not improve on any outcome measure.
Semantic Feature Analysis (SFA)
A study 7 including one person with Wernicke’s aphasia showed gains on treated items with some generalization, but no change in word retrieval in discourse following treatment using Semantic Feature Analysis.
Communication Partner Training (CPT)
Communication partner training is often the first and most effective treatment to establish communication and begin building rapport with a person with Wernicke’s aphasia. Partners often need to be trained to ignore the actual words or nonwords and focus on the facial expressions, gestures, and intonation of the person speaking fluent jargon.
Using written keywords can make a huge difference in comprehension and give the person with Wernicke’s aphasia a physical referent when wanting to return to a topic. Many of the studies done on CPT have included people with fluent aphasia, with some specifying Wernicke’s type, with positive results. 8
Intensive Therapy
A treatment study 9 from 2015 compared two kinds of intensive therapy for people with fluent aphasia. Six of the nine subjects had Wernicke’s aphasia. After more than 20 hours of therapy in 2 weeks, 2/3rds of the subjects improved significantly on measures of everyday communication, including 5 of the 6 with Wernicke’s aphasia. Both a lexical-semantic treatment (BOX) and a communication-focused treatment (CIAT) were used, with minimal differences in outcomes.
One study 10 looked at intensive naming therapy for a person with chronic Wernicke’s aphasia. After 2 weeks of Constraint-Induced Aphasia Therapy and 2 weeks of PACE, all treated words improved, with 75% of the words learned under CIAT retained at 6 months post-treatment (vs. 33% of PACE words). Untreated words did not improve.
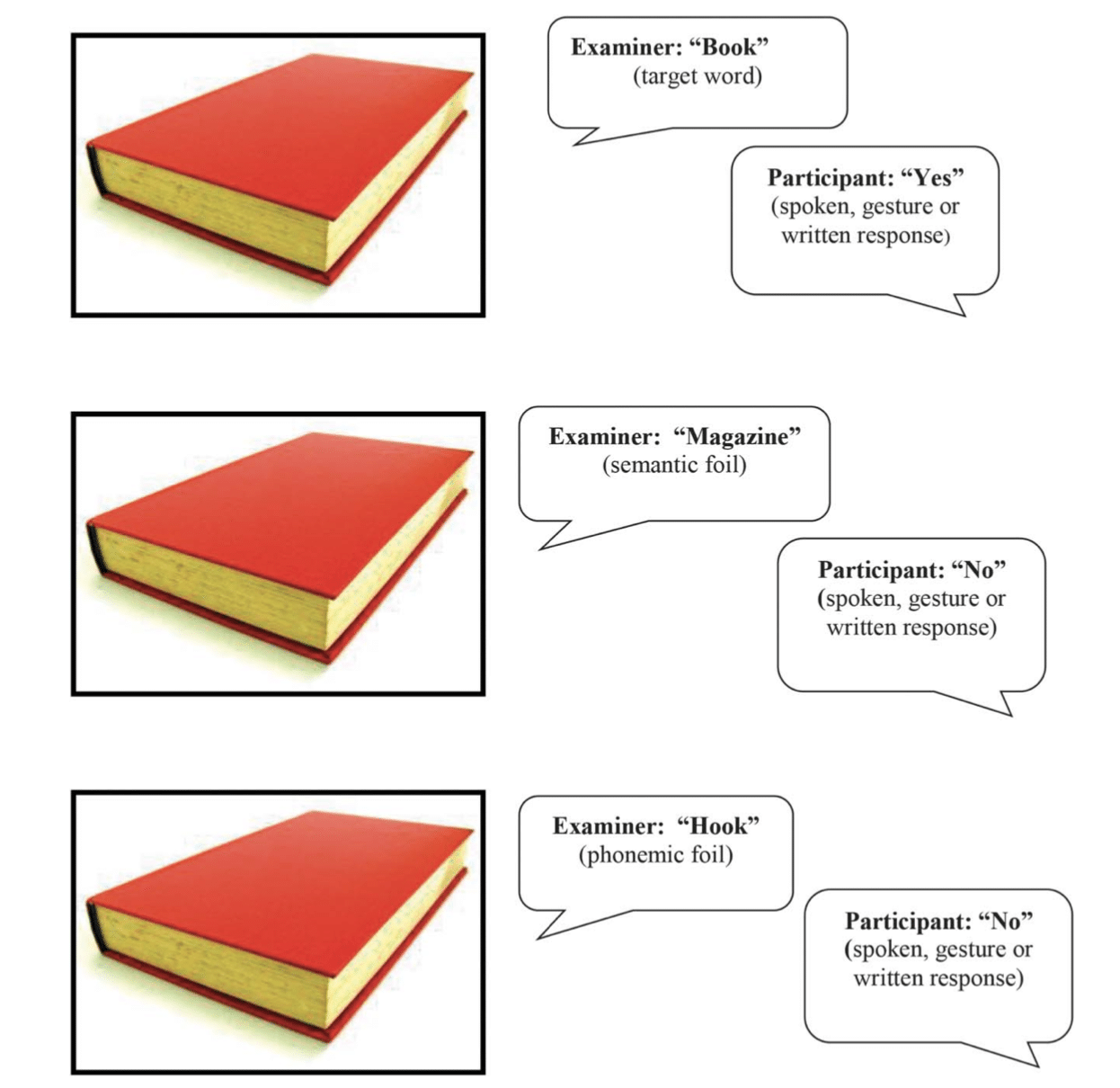
Another study by Knollman-Porter et al. 11 looked into intensive therapy for auditory comprehension. One of the two subjects had severe fluent aphasia. A yes/no task was delivered intensively (40 hrs in 4 weeks) using high-frequency nouns (e.g. “is this a cat?” showing a picture of a cat, dog, or hat). The participant with fluent aphasia started at 16% accuracy and reached a high of 84% accuracy. She averaged 68% accuracy at the end of the trial, and maintained 66% after the treatment ended. Most notably, she showed 62% accuracy for untreated words, showing generalization.
Woodhead et al. 12 studied 20 people with auditory comprehension challenges, 11 of which had Wernicke’s aphasia. After 50 hours of Earobics® software training in 5 weeks, speech comprehension improved to a level of statistical significance, but still only a small improvement. This is important nonetheless, as Wernicke’s aphasia can be so difficult to treat, so even a small improvement is a good sign, and using (formerly) commercially-available software to deliver therapy is a viable way of achieving the intensity used in the study.
Learning more about Wernicke’s Aphasia
Dr. Jane Marshall gives a wonderful overview of jargon aphasia in her chapter in Aphasia Rehabilitation: Clinical Challenges. *Amazon affiliate link
The full chapter on Jargon Aphasia is available for you to read for free here.
While Dr. Marshall’s chapter on jargon aphasia seems a bit grim with many treatments that fail to show a response or generalize, she wraps it up with an optimistic message that using conversation partner training, along with pairing written keywords with conversation (as is taught in Supported Conversation with Adults with Aphasia), can be an effective gateway into more familiar speech therapy that begins with setting goals, selecting a treatment plan, delivering therapy, and measuring outcomes. We simply need to know more about which treatments help with the jargon symptoms of Wernicke’s aphasia.
Learn more about what Wernicke’s aphasia is and what it looks like in this article with a viral video of stroke survivor Byron Peterson speaking with Tactus Therapy co-founder Megan Sutton.
What is Fluent Aphasia?
Fluent aphasia is a disorder with effortless but largely meaningless speech. Learn what it is, see a video, and find out how to help Wernicke’s-type aphasia.
4 min read
Notes on diagnosing Wernicke’s Aphasia
A diagnosis of Wernicke’s aphasia requires poor comprehension, poor repetition, and relatively effortless but empty speech made up of words and non-words (neologisms or paraphasias) that is referred to as jargon or “word salad”. Poor insight/awareness and talking over people (press of speech) are also common.
Here’s a really good rule of thumb for all speech pathologists to remember:
Fluent aphasia rarely, if ever, co-exists with apraxia of speech.
The inability to repeat seen in people with Wernicke’s aphasia is a repetition impairment, not a motor speech impairment. Even if you notice oral groping behaviors, that doesn’t make it verbal apraxia. Use the Apraxia of Speech Rating Scale (ASRS) to determine the presence of apraxia with non-fluent aphasia – it just won’t be there if the aphasia is fluent.
It’s also good to remember that if you hear near-normal prosody used on a repeated single syllable, word, or phrase, it is likely a stereotypee or stereotyped utterance common in global aphasia. For a true Wernicke’s aphasia, you will hear a variety of sounds, non-words, and words that create jargon.
Measuring Fluency
Aphasia is often divided into two types: fluent and non-fluent. So how do we know which is which? Fluency can be measured in many ways, as it is a multi-dimensional quality of speech and somewhat subjective in its measurement. 13
Single measures: In the Aphasia Diagnostic Profiles assessment (ADP), fluency is determined by the longest average phrase length on discourse tasks. A ratio of 5+ word phrases to 1-2 word phrases has also been used to separate fluent from non-fluent. Even calculating the rate of speech in words or syllables per minute may give clinicians a good idea of fluency.
Multidimension measures: The BDAE-3 standardized assessment uses rating scales of six dimensions of speech: melodic line, phrase length, articulation, grammaticality, paraphasia, and word-finding ability. The WAB-R assessment battery uses a fluency scale of 11 descriptors from 0=“no words or short, meaningless utterances” to 10=“sentences of normal length and complexity without definite slowing, halting, or paraphasias.” Scores of 5 and above are considered fluent.
Clinician perception is perhaps the most widely-used measure, though there is not a high degree of inter-rater reliability. In a study looking at clinical judgment of fluency, “speech productivity”, or the amount of time spent speaking compared to pause time, seemed to be the most important factor. Efforts are underway to develop a better system of measuring and determining fluency. 14
Download a “How To” guide now!
Get your free PDF handout of How To Do Treatment of Wernicke’s Aphasia (TWA). Includes a printable data tracking sheet to use in therapy!
In addition to receiving your free download, you will also be added to our mailing list. You can unsubscribe at any time. Please make sure you read our Privacy Policy and Terms & Conditions.
References:
- Pedersen, P. M., Vinter, K., & Olsen, T. S. (2004). Aphasia after stroke: type, severity and prognosis. Cerebrovascular Diseases, 17(1), 35-43. (Full-Text PDF)
- Marshall, J. (2010). Classification of aphasia: Are there benefits for practice?. Aphasiology, 24(3), 408-412.
- Yagata, S. A., Yen, M., McCarron, A., Bautista, A., Lamair-Orosco, G., & Wilson, S. M. (2017). Rapid recovery from aphasia after infarction of Wernicke’s area. Aphasiology, 31(8), 951-980. [Full-Text HTML]
- Edmonds, L. A. (2016). A review of Verb Network Strengthening Treatment: Theory, methods, results, and clinical implications. Topics in Language Disorders, 36(2), 123-135. (Full-Text PDF)
- Lerman, A., Goral, M., Edmonds, L. A., & Obler, L. K. (2020). Measuring treatment outcome in severe Wernicke’s aphasia. Aphasiology, 34(12), 1487-1505.
- Rogalski, Y., Edmonds, L. A., Daly, V. R., & Gardner, M. J. (2013). Attentive Reading and Constrained Summarisation (ARCS) discourse treatment for chronic Wernicke’s aphasia. Aphasiology, 27(10), 1232-1251.
- Boyle, M. (2004). Semantic feature analysis treatment for anomia in two fluent aphasia syndromes. American Journal of Speech-Language Pathology, 13(3), 236-249.
- Simmons-Mackie, N., Raymer, A., & Cherney, L. R. (2016). Communication partner training in aphasia: An updated systematic review. Archives of Physical Medicine and Rehabilitation, 97(12), 2202-2221.
- Wilssens, I., Vandenborre, D., van Dun, K., Verhoeven, J., Visch-Brink, E., & Mariën, P. (2015). Constraint-induced aphasia therapy versus intensive semantic treatment in fluent aphasia. American Journal of Speech-Language Pathology, 24(2), 281-294. [Full-Text PDF]
- Kurland, J., Baldwin, K., & Tauer, C. (2010). Treatment-induced neuroplasticity following intensive naming therapy in a case of chronic Wernicke’s aphasia. Aphasiology, 24(6-8), 737-751.
- Knollman-Porter, K., Dietz, A., & Dahlem, K. (2018). Intensive auditory comprehension treatment for severe aphasia: A feasibility study. American Journal of Speech-Language Pathology, 27(3), 936-949.
- Woodhead, Z. V., Crinion, J., Teki, S., Penny, W., Price, C. J., & Leff, A. P. (2017). Auditory training changes temporal lobe connectivity in ‘Wernicke’s aphasia’: a randomised trial. Journal of Neurology, Neurosurgery & Psychiatry, 88(7), 586-594. [Full-Text PDF]
- Clough, S., & Gordon, J. K. (2020). Fluent or nonfluent? Part A. Underlying contributors to categorical classifications of fluency in aphasia. Aphasiology, 34(5), 515-539. [Full-Text PDF]
- Gordon, J. K., & Clough, S. (2020). How fluent? Part B. Underlying contributors to continuous measures of fluency in aphasia. Aphasiology, 34(5), 643-663. [Full-Text PDF]
This article is by no means intended to be a systematic review of the literature. It is meant to be clinically useful for speech-language pathologists looking for treatment direction. We hope it helps you to help others.