5 Things I Didn’t Understand about the Life Participation Approach to Aphasia (LPAA)
7 min read
Have you heard of the Life Participation Approach to Aphasia (LPAA)? Did you know there’s a whole new organization focused on this approach? After learning about AphasiaAccess and their mission to serve as a professional organization for LPAA providers, I decided to attend their first conference held last week in Boston. It was one of the most powerful conferences I have ever been to, filled with the top experts in the field and over 150 people genuinely passionate, motivated, and excited about what they are doing.
As an inpatient speech-language pathologist (SLP) working in rehab, I didn’t think the life participation approach was for me. I thought it was something used only by aphasia centers for people with chronic aphasia who had largely plateaued in their language recovery. My patients wanted to get better. My patients were too early in their stroke rehab to want to join an aphasia book club or focus only on ordering in a restaurant.
Here are 5 lessons I learned about life participation therapy that I hope other SLPs will benefit from as well:
1) LPAA is Not Anti-Impairment Therapy
The Life Participation Approach to Aphasia is not against, or even an alternative to, impairment-based therapy; it encompasses and expands on it to include all areas of a person’s life. Therapy looks at the language impairment and treats it, but also examines the environmental barriers and facilitators, personal identity and emotions, and participation in daily life.
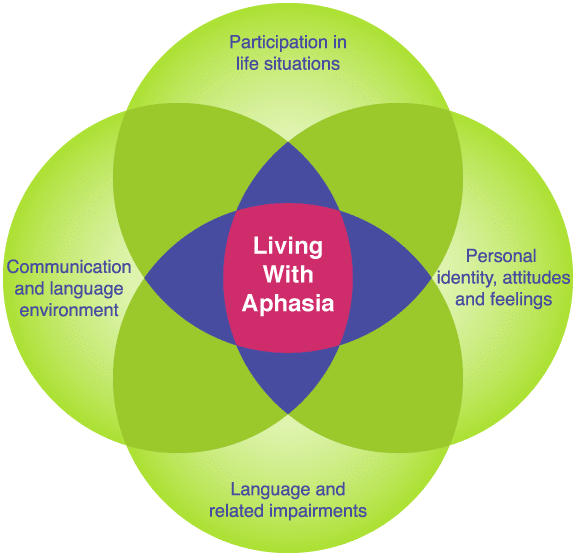
What good is a complete sentence if you’re too depressed to leave your home? Why learn to use gestures if you have no friends to talk to? Why is only the person with aphasia treated when others around them are also affected? Conversely, what good is a positive environment if a person has no communication skills to interact with it? They all go together.
2) You Might Already Be Doing LPAA
I always did my best to provide education to my patients and their families about aphasia and stroke. I counseled them through the grief and loss of function and independence. I spent sessions training care partners and staff on the best strategies to use to help my patients communicate more easily and express their opinions. I put pictographic signs up around the unit to make it easier for my patients to find their way around. I set goals for them to understand their medications and use their strategies in recreational groups. I did all of this along with describing pictures, copying words, expanding sentence length, and reading aloud in unison – all evidence-based therapy methods for remediating language in aphasia.
I was doing LPAA, but I didn’t know it! Well, I was mostly doing LPAA. When I look back, there was more I could have been doing and ways I could have made it all tie together better. But I was under the misconception that LPAA wasn’t the approach I should be taking because I needed to do therapy with the goal of improving language. I couldn’t have been more wrong.
3) LPAA is a Non-Prescriptive Approach
LPAA is not a procedure you must follow, or even a therapy method at all. You select the activity-based goal, and then choose which treatment methods you want to use to get there. You might pick semantic feature analysis to improve word finding in conversation with family; anagram and copy therapy to improve writing for making shopping lists; or scripting to increase ability to start conversations at the community center. Nearly any treatment method can be customized to fit in with the life participation approach.
How it Works: First you pick the end goal that ties into life with aphasia, and work backwards. If the goal is to send emails to family members, you might choose to get there by working on writing letters of the alphabet, then writing words, phrases, and sentences. Alternately, you may choose to get to the same goal of sending emails by using a bank of phrases the person can copy and paste into their message.
As a highly educated and skilled professional, the SLP is able to decide the best approach to reach the participation goal. You can work on the impairment, modify the immediate or community environment, or address the attitude of the person/family (through counseling, motivational interviewing, or education) – or do all three.
This is why I started creating apps like Language Therapy and Category Therapy. I didn’t want to spend my time with patients with aphasia doing repetitive drills, even though I knew that repetition was essential for neuroplasticity. I wanted to use my skills to do more skilled therapy. I wanted to send them home with exercises, after training everyone involved, and then focus on the things an app can’t do in our sessions, like conversation, counseling, and problem-solving barriers.
4) Quality of Life is the Ultimate Goal
Compared to impairment-based treatment, participation-focused therapy is far less likely to show plateaus in progress. Because participation is the goal, we can still make progress even if the client’s language isn’t improving.
Communication is more than just information transfer; it is a social action that requires:
- language
- opportunity
- activities or context
- a good communication partner
- the confidence to try
Speech therapy can address all of these things if we do it correctly. These elements of communication should be the things we write into our therapy goals. People with aphasia and their families also need information on aphasia, stroke, and treatment options – not just once, but early and often for it to sink in and adapt as they improve.
Our clients will have greater buy-in to achieving the goals that matter to them. There will always be new goals to work on as the person re-engages in life and wants to do more. When we involve the person with aphasia and their family in setting goals, we know our efforts are not wasted since they are getting what they want out of therapy, and we feel good for providing effective and satisfying treatment.
5) Life Participation Therapy Can Start Now
Great news! You can start using the LPAA today. No matter the setting, all clients with aphasia have activities they need to participate in. It just takes thinking about things more holistically as you write truly functional treatment goals.
Every stage of the therapy process has participation goals if you look for them. The first day in acute care, there are loved ones who need education. There is a patient who needs to be safe and feel competent. Communicating with family members, understanding and making medical decisions, and being safe in the hospital environment are all early goals for intervention. In a rehab setting, work can expand to participation goals such as selecting from a menu, managing the therapy schedule, or making discharge decisions – all of which can be achieved while language improves in the process.
With length of stay steadily decreasing (3-4 weeks of inpatient care is now typical in many areas), the inpatient therapists are less likely to see their clients through to the end goal. However, they are in an ideal position to set the groundwork for a positive relationship between clients/families and speech therapy, and provide the resources, referrals, and tools needed for the coming months or years of recovery.
It might be more efficient to spend time training clients to use technology and apps, rather than only drilling language exercises, so when those clients are discharged, they have options for continuing to practice language skills and connect with others. Without these resources, they may improve while with us, but then return home with no activities other than watching TV. Referrals to outpatient therapy, community stroke or aphasia groups, and educational and technical resources can mean the difference between existing with aphasia and living well with aphasia.
Life Participation Approach to Aphasia Therapy
The LPAA is not really an approach to aphasia therapy, it is the approach. Anyone doing therapy that only addresses language impairment may be doing a disservice to their clients. It’s relatively easy to switch your mindset to consider the whole person, their environment, and the connection of therapy tasks to participation in the activities of daily life.
Impairment-based therapy is an important and effective tool for helping people with aphasia to improve. Just be sure your toolbox also includes education, partner training, counseling, and environmental modifications to ensure your clients can truly benefit from your efforts and participate in their lives.
Thank you to Nina Simmons-Mackie, Aura Kagan, and Roberta Elman for presenting the information summarized here at the inaugural AphasiaAccess leadership summit. Also, a very heartfelt thank you to Audrey Holland for telling me I “better be there” at the conference and for her wisdom and inspiring work in the field.
